Unlike large institutions with full IT teams and infrastructure, Dr. Ryan operates in an environment where cloud storage and external data sharing are highly restricted. Yet, with Medicalholodeck, he’s built a streamlined, compliant setup that allows him to plan surgeries in full 3D - right from his office.
Building a local, VR-ready workflow
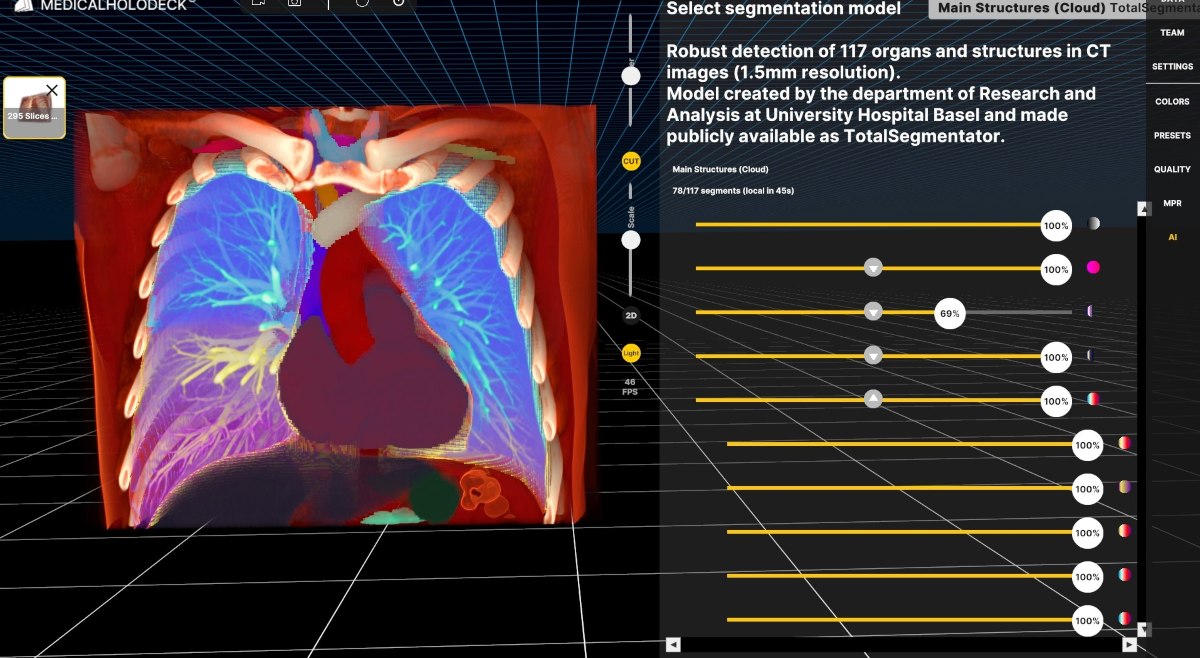
Early on, Dr. Ryan tested the limits of Medicalholodeck, aiming to break the system and understand how far it could be pushed. Today, he runs a highly optimized workflow using a local network setup: wireless VR headsets (Meta Quest), laptops connected to a dedicated router, and local SSD storage for scan data.
Each VR headset connects through a virtual desktop app to a paired PC. In under five minutes, he can move from scan access to immersive surgical planning - completely offline. This approach ensures speed, security, and independence.

Mark Ryan, MD, MSPH, FACS is a board-certified pediatric surgeon and Assistant Professor of Surgery at the University of Missouri–Kansas City School of Medicine. He currently serves as Director of Surgical Critical Care at Children’s Mercy Kansas City, where he specializes in complex surgical procedures and intensive care for critically ill children.
With dual training in public health and surgery, Dr. Ryan brings a systems-based approach to clinical care and surgical planning. He is especially interested in integrating advanced technologies into everyday workflows - including virtual reality (VR) for preoperative planning, surgical education, and patient communication.
From volume rendering to surgical strategy
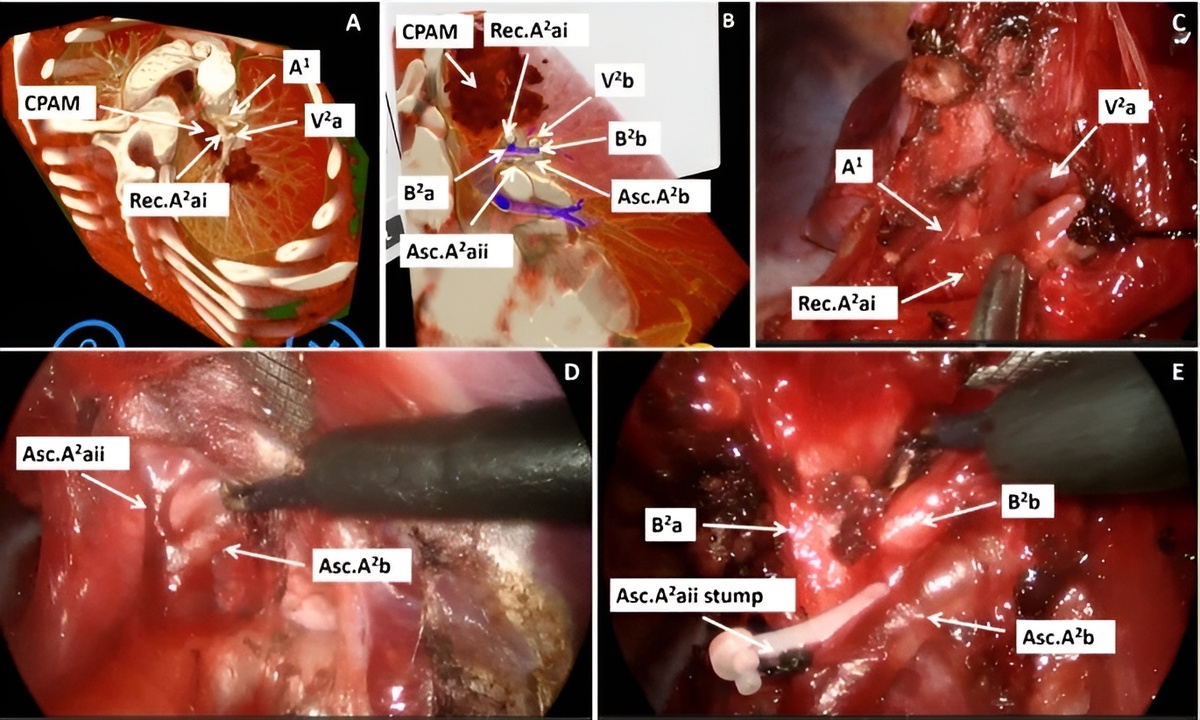
Using Medicalholodeck, Dr. Ryan transforms standard DICOM scans into 3D visualizations that allow him to explore anatomy from every angle. He emphasizes the value of AI-powered segmentation, which helps him identify key structures without having to model everything manually. These segmented models serve as landmarks - especially useful when navigating complex anatomy like the portal vein or vascular structures near tumors.
In one example, he describes planning a stapler approach to a pancreatic mass. Being able to previsualize the vascular window in VR gave him confidence and clarity - something traditional imaging alone couldn’t provide.
Real cases, real impact
From thoracic surgery to liver cyst resections, Dr. Ryan demonstrates how VR enhances anatomical understanding. He shows how segmentations, volume renderings, and translucent overlays help distinguish tissues of similar densities - especially in low-contrast regions like the abdomen.
Patient impact and future vision
VR isn’t just helping surgeons - it’s changing how patients experience care. Dr. Elsayed notes that when patients see their own pathology in VR, their understanding improves dramatically. He also sees Medicalholodeck playing a vital role in global education through a future RxR surgical atlas: a shared VR library of recorded surgeries that can train clinicians anywhere in the world.
He also highlights the use of Medicalholodeck’s tools to measure tumors, define resection margins, and adjust visualization settings for clearer planning. In pediatric and adolescent cases, where anatomy can vary significantly, this level of detail makes a measurable difference.
Looking ahead: AR, templates, and education
Dr. Ryan is also thinking about what’s next. He’s eager to explore planning templates and augmented reality (AR) integrations - tools that could further streamline his preoperative process and enhance intraoperative guidance.
He sees potential not only in planning but in education - both for trainees and patients. By turning complex imaging into something you can literally walk around and examine, VR is reshaping communication and understanding in medicine.
For more information, contact info@medicalholodeck.com March 2025