Acknowledging real-world challenges - such as physician shortages, limited computing infrastructure, and mixed user comfort with headsets - they asked a simple but important question: How can immersive imaging be made more practical, accessible, and scalable? Their answer: bring 3D imaging directly to smartphones and tablets.
A scalable, device-agnostic solution
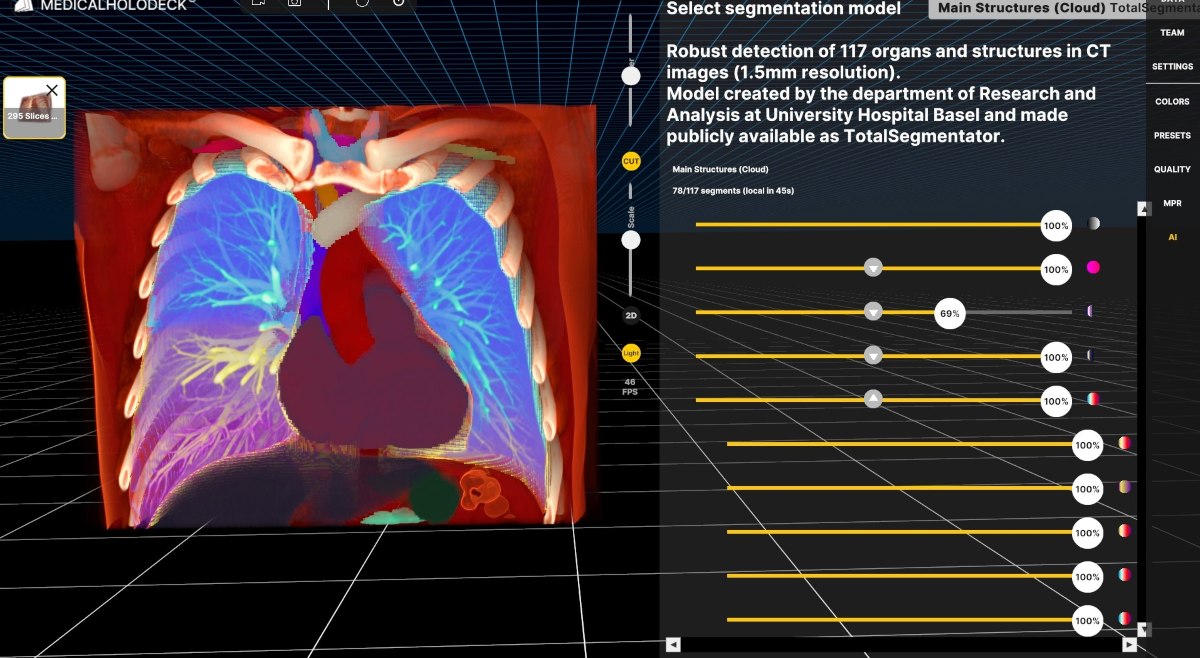
With billions of smartphones now in use - many outperforming standard laptops - the Bonn team developed a solution that enables one-click access to XR imaging via mobile devices. This opens 3D visualization to a wide audience: not only radiologists, but all healthcare providers and even patients.
Integrated with Medicalholodeck, this solution is already in use across four key areas:
-
Medical education – Tablet-based radiology teaching using real CT/MRI cases
-
Patient communication – Interactive XR views of pathology for better understanding
-
Clinical planning – Immediate 3D reconstruction in emergency or interventional settings
-
Interdisciplinary collaboration – Integration of non-radiological datasets like microscopy

Prof. Dr. med. Daniel Kütting is a senior consultant at the Department of Diagnostic and Interventional Radiology at University Hospital Bonn, Germany. He leads the sections for Cardiothoracic Imaging and Interventional Radiology and oversees the CT division. His clinical and academic work focuses on advanced imaging techniques, including cardiac imaging, 3D visualization, and interventional procedures.

Dr. Alexander Böhner is a radiologist at the Department of Diagnostic and Interventional Radiology at University Hospital Bonn, Germany. His work focuses on diagnostic imaging, with particular interest in integrating innovative technologies into clinical practice. Dr. Böhner is actively engaged in applying extended reality (XR) tools for radiological visualization, patient communication, and medical education.
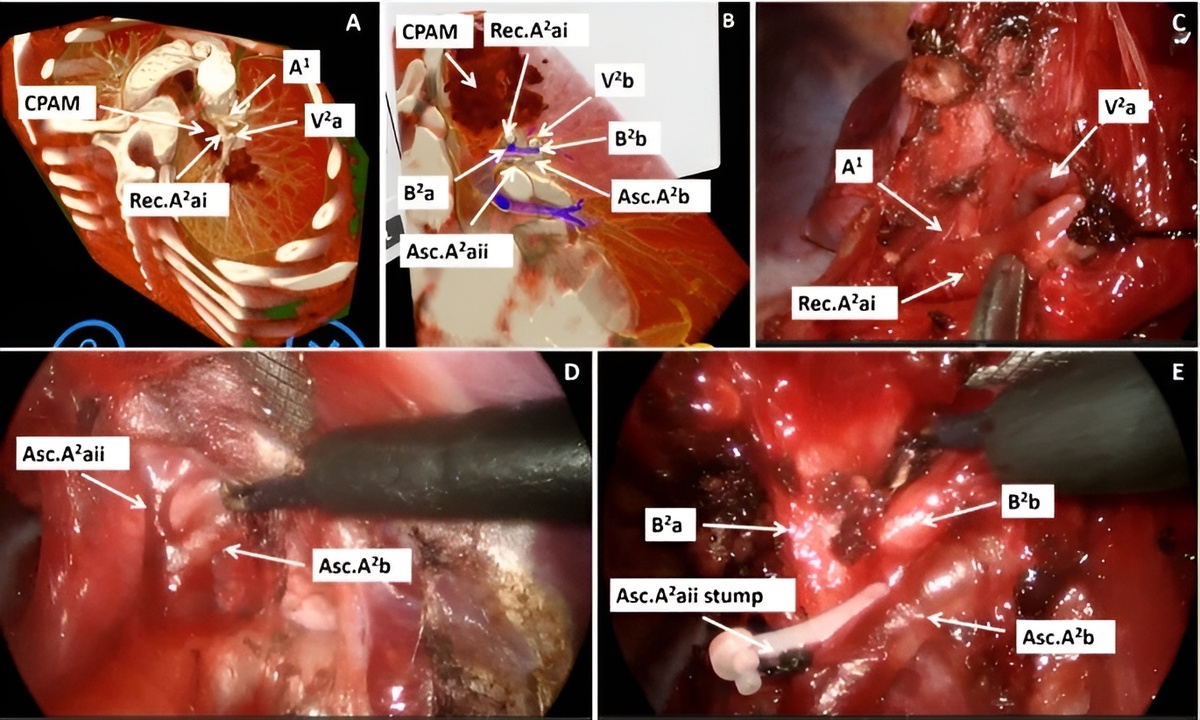
Clinical use cases and impact
Several examples highlighted the practical value of this mobile XR workflow. A student uses CT-based models to locate renal cysts during ultrasound. In emergency care, trauma or dissection scans are reconstructed in minutes and reviewed bedside in 3D on an iPad.
In interventional radiology, 3D views helped identify optimal access to treat a complex pseudoaneurysm. For oncology patients undergoing PET/CT, 3D fusion imaging was used to communicate therapy progress - helping patients better understand their treatment journey.
Engaging patients and students
Feedback from patients and students has been highly encouraging. Over 90% of patients preferred XR-based visualization over traditional grayscale images. Medical students also reported enhanced comprehension and engagement during tablet-based learning sessions.
With low data burden and a highly intuitive interface, the team refers to this approach as "democratized imaging" - a practical, scalable solution suitable for hospitals of any size or resource level.
Looking ahead
Prof. Dr. Kütting and Dr. Böhner emphasized that mobile XR is not a compromise - it’s a strategic evolution of how we engage with imaging. As they continue evaluating outcomes, they envision expanding access, improving interdisciplinary collaboration, and empowering patients through better visualization.
This work redefines what XR can look like in medicine: accessible, fast, and meaningful - not just for specialists, but for every user across the healthcare spectrum.
For more information, contact info@medicalholodeck.com March 2025