Dr Tidbury’s academic foundation lies in orthoptics and vision research, with a focus on how depth perception is processed in the brain - even among individuals who are technically stereo blind. His early work explored alternative visual mechanisms, such as motion and monocular cues, that can still generate a strong sense of depth. These insights led to a broader interest in how clinicians perceive complex anatomy from imaging data - and how those perceptions can be enhanced using immersive tools.
Bringing medical imaging to life with VR
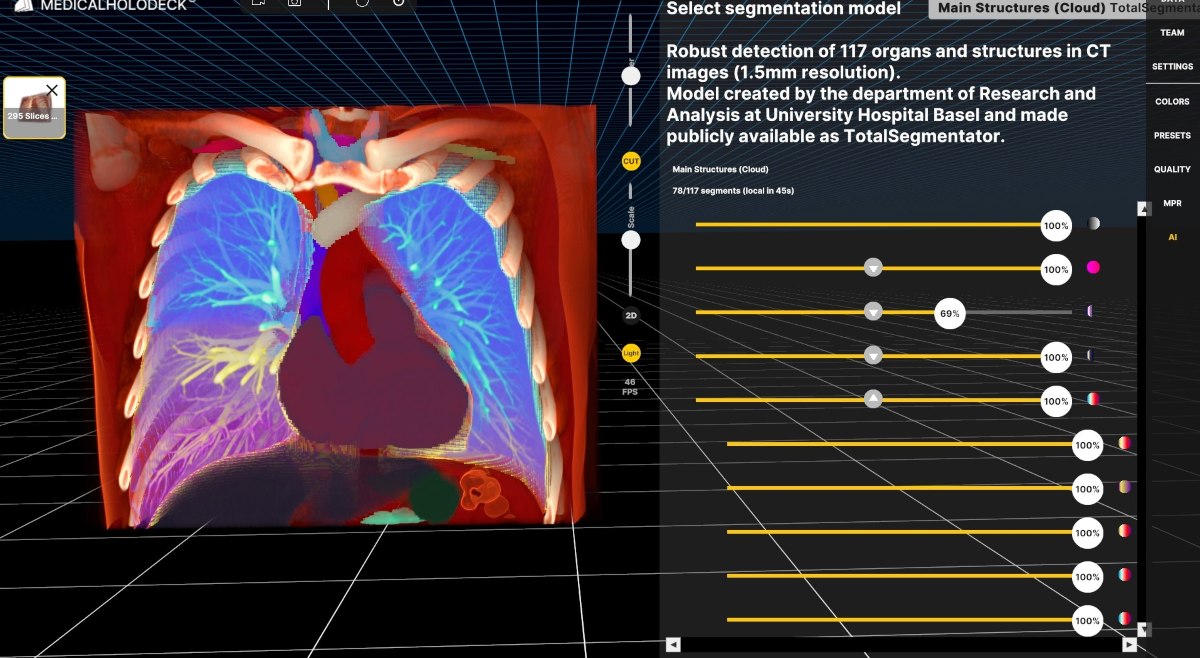
At Liverpool Heart and Chest Hospital, Dr Tidbury implemented Medicalholodeck, a stereoscopic VR platform for visualizing DICOM data and 3D anatomical models. This technology allows clinicians to view scans in a fully immersive environment - seeing anatomy not just in three dimensions, but with the spatial fidelity that mirrors real-life perception.

Dr Laurence Tidbury is the Research IT System Lead at Liverpool Heart and Chest Hospital NHS Foundation Trust, UK. With a PhD in Vision Science and a background in Orthoptics, his work bridges clinical research and technology, focusing on visual perception and medical imaging.
He applies virtual reality tools like Medicalholodeck to enhance 3D visualization of patient anatomy, supporting surgical planning and improving clinical outcomes through immersive, stereoscopic viewing.
Cardiac case: virtual models vs. 3D printing
In one cardiac surgery case, a patient presented with a rare single-ventricle defect and dextrocardia. The surgical team needed a 3D model to plan the procedure, but the cost of 3D printing (approximately £1,700) was a barrier.
Instead, Dr Tidbury prepared a VR-based model using Medicalholodeck. The team was able to explore the heart virtually, gaining the same anatomical understanding without the logistical delay or expense. This approach proved not only cost-effective but also clinically valuable.
When depth perception changes the plan
Another notable example came from anesthesiology. A patient with a difficult tracheal anatomy required a tailored intubation approach. Using CT data, Dr Tidbury created a virtual model of the airway. Once viewed in VR, the anesthetist could clearly assess the twists, narrowing, and spatial orientation - details that were difficult to interpret from axial slices alone. This kind of immersive viewing helped inform the clinical strategy, reducing risk and improving procedural confidence.
More than a gimmick: A clinical necessity
While 2D imaging offers convenience, it also introduces perceptual limitations. Flat screens rely heavily on monocular depth cues and can create visual conflict when viewed with both eyes. In contrast, stereoscopic displays provide each eye with a unique perspective - matching how the brain naturally interprets depth and spatial relationships.
Dr Tidbury shared one instance where stereoscopic visualization led to a critical change in surgical planning. A consultant, after reviewing a VR model of calcified cardiac tissue, recognized that its orientation differed from what was initially assumed. Had the original plan been followed, it might have led to a non-recoverable complication.
Toward a formal imaging service
Building on these successes, Dr Tidbury is working to establish a formal VR-based imaging review service within the Trust. The goal is to integrate immersive viewing into routine clinical workflows, particularly for complex cardiothoracic cases and pre-operative planning. For Dr Tidbury, this is not about novelty - it’s about giving clinicians the perceptual tools they need to make better-informed decisions.
Conclusion: A case for immersive imaging
Dr Tidbury’s work highlights an important lesson: technology should align with how the brain works. Stereoscopic viewing - especially in virtual reality - does exactly that. By providing a more naturalistic and immersive way to interpret medical images, it enhances anatomical understanding, supports decision-making, and in some cases, directly impacts patient outcomes.
As immersive technologies mature, their role in medicine will only expand. Dr Tidbury’s experience shows that stereoscopic imaging isn’t just beneficial - it’s becoming essential.
For more information, contact info@medicalholodeck.com March 2025