Lacrimal Sac Reconstruction With Virtual Reality
Virtual Reality and Telemedicine in Endoscopic Procedures for Treatment of Lacrimal Drainage Obstruction
Rafal Nowak, MD, PhD
Department of Ophthalmology, Military Institute of Medicine, Warsaw,
Poland
Correspondence to:
Publication
Case
A female of 43 years presented to the lacrimal clinic with a history of slow growing lesion at the inner angle of the left eye associated with epiphora of 5 years. The swelling was not associated with any discharge, pain, or acute infections in the past.
Nasolacrimal duct obstruction is routinely treated with the surgical procedure of dacryocystorhinostomy (DCR), which refers to the creation of a functional pathway for tears to drain into the nasal cavity by means of making an osteotomy and opening the lacrimal sac directly into the nasal cavity. It can be performed via an external or endonasal approach. DCR that has failed multiple times is uncommon and poses a surgical challengeIV. Unsuccessful dacryocystorhinostomy may result from chronic inflammatory changes in the nasal cavity, which are often found during GPAV.
Clinical examination revealed a left-sided firm, well-defined lesion in the area of the lacrimal sac fossa. Lacrimal irrigation was suggestive of a partial nasolacrimal duct obstruction. The right-side examination was normal. Different modalities of imaging were performed, including dacryocystography (DCG), computed tomography dacryocystography (CT-DCG) and magnetic resonance imaging (MRI)(Fig.1).

Figure 1. MRI shows a well-defined lesion (cyst) in the left lacrimal fossa (red arrow)
Medical Imaging XR (Medicalholodeck AG, Zurich, Switzerland) three-dimensional reconstructions obtained from CT-DCG DICOM files showed a well-defined lesion in the left lacrimal sac fossa, extending up to the beginning of the nasolacrimal canal (bony). The lacrimal sac appeared to be compressed against the posterior wall of the lacrimal fossa (Fig. 2-4).
Nasal endoscopy examination was normal other than a deviated septum. Further 3D-dimensional reconstructions were performed from the CT-DCG data using the Meshlab (Visual Computing Lab, CNR-ISTI, Pisa, Italy) and Blender software tools (Blender Foundation, Amsterdam, Netherlands).
The reconstructions showed the intricate relationship of the lesion with the compressed lacrimal system (Fig. 5). The surgical plan was a careful excision.
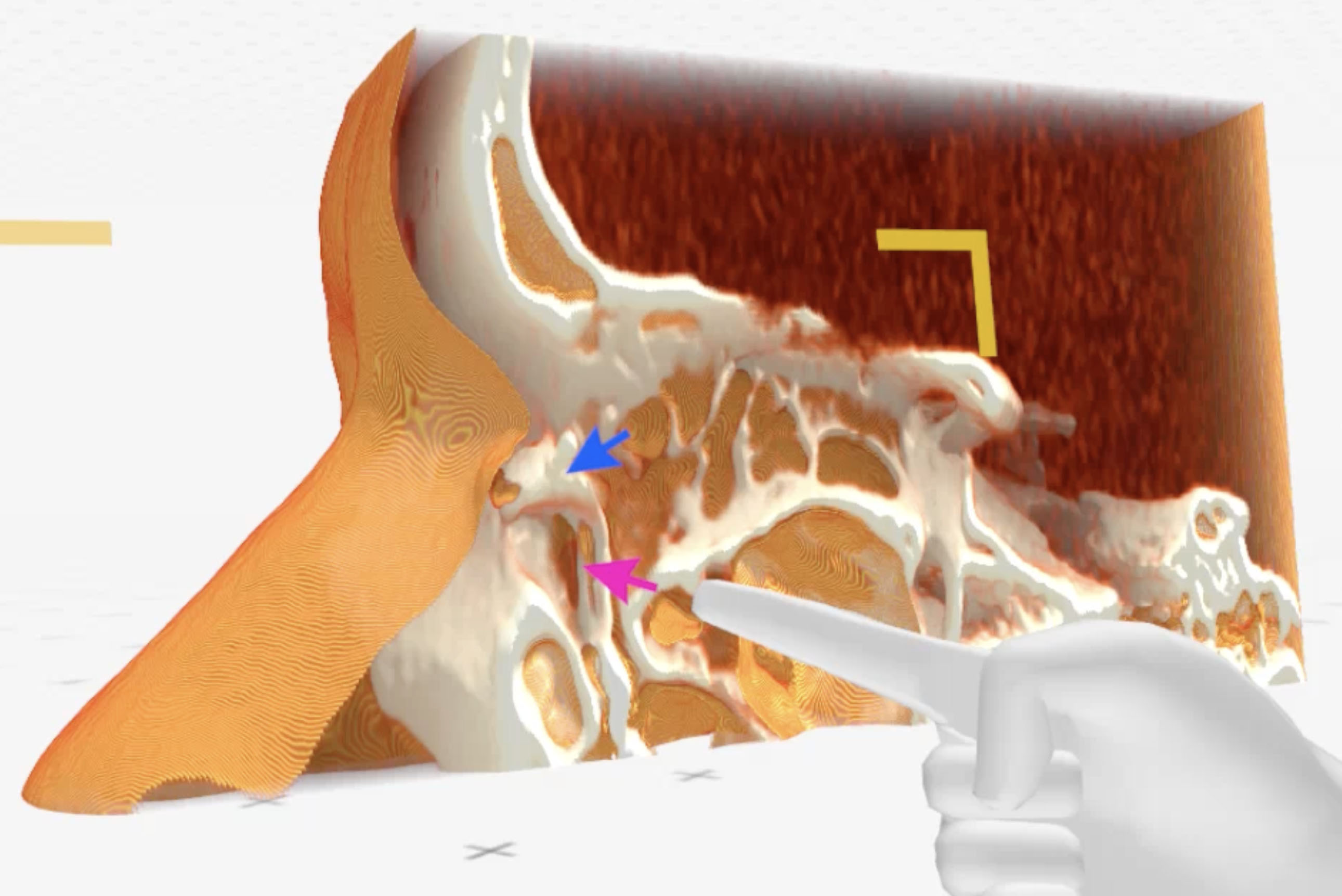
Figure 2. Medical Imaging XR reconstruction shows contrast dye in the left lacrimal passages (blue arrow) and a space referring to a lesion compressing the lacrimal sac (pink arrow)
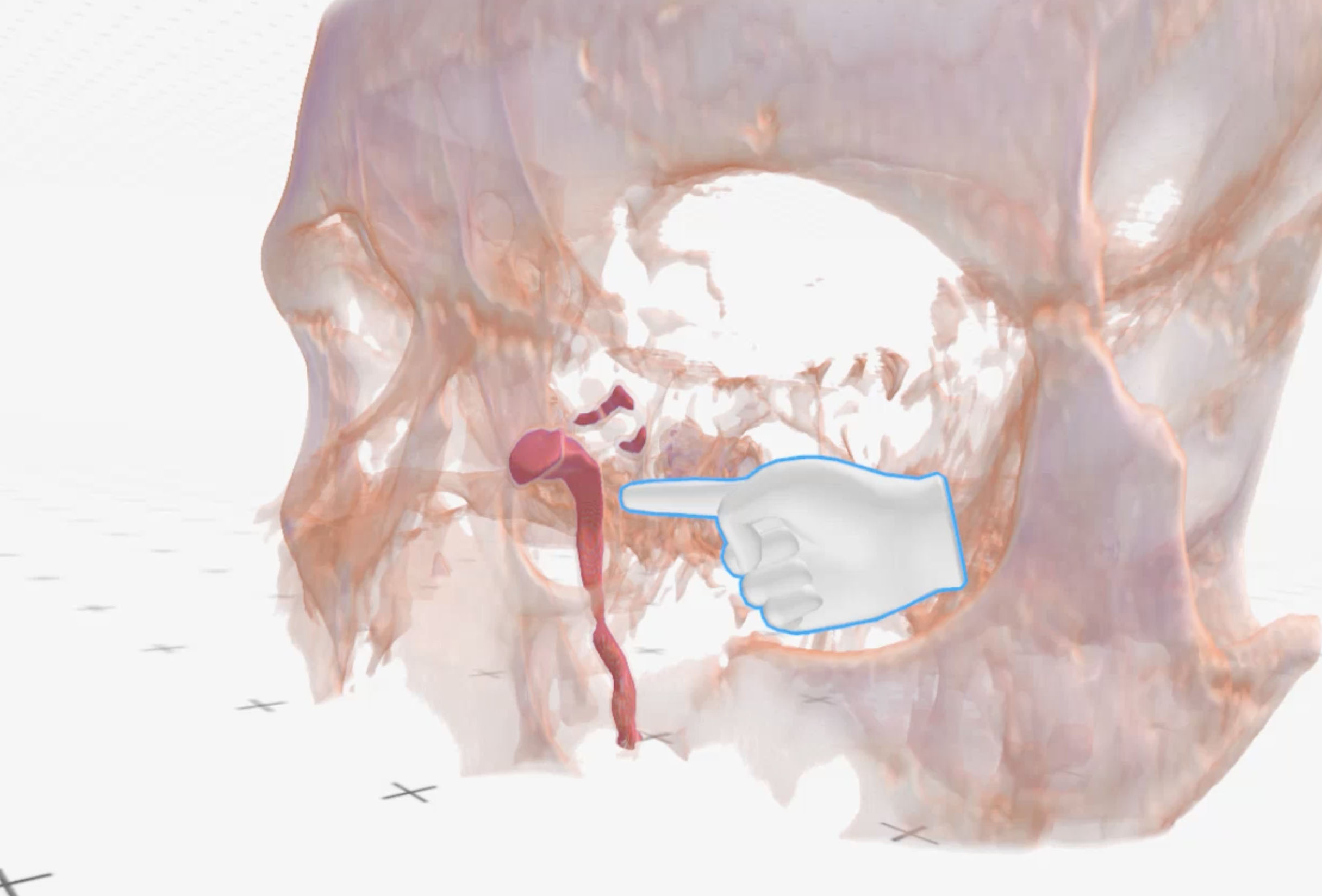
Figure 3. Medical Imaging XR reconstruction shows isolated contrast dye in the left lacrimal passages (red) and significantly compressed lacrimal sac
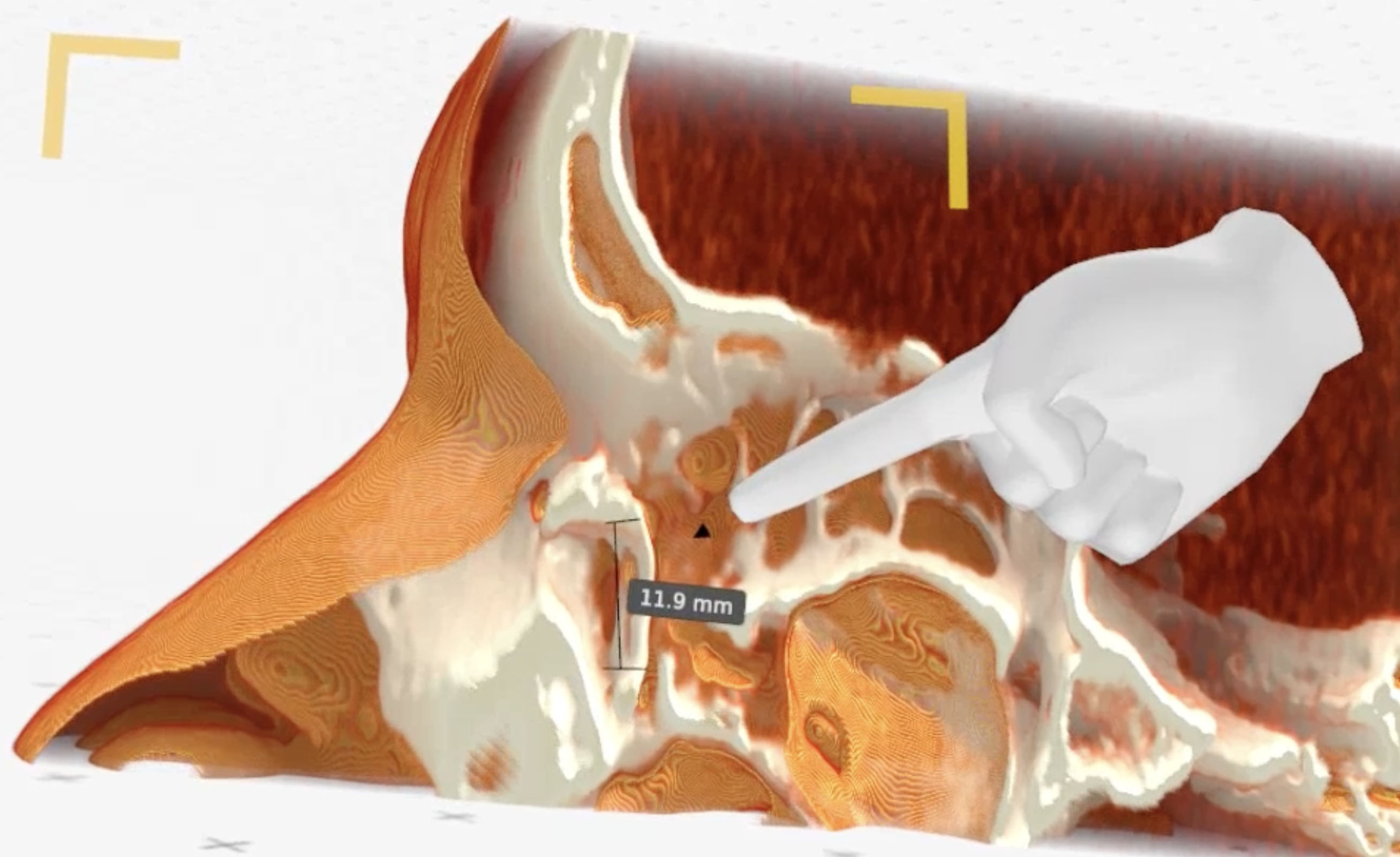
Figure 4. Medical Imaging XR reconstruction shows vertical dimension of the cyst (11.9mm)
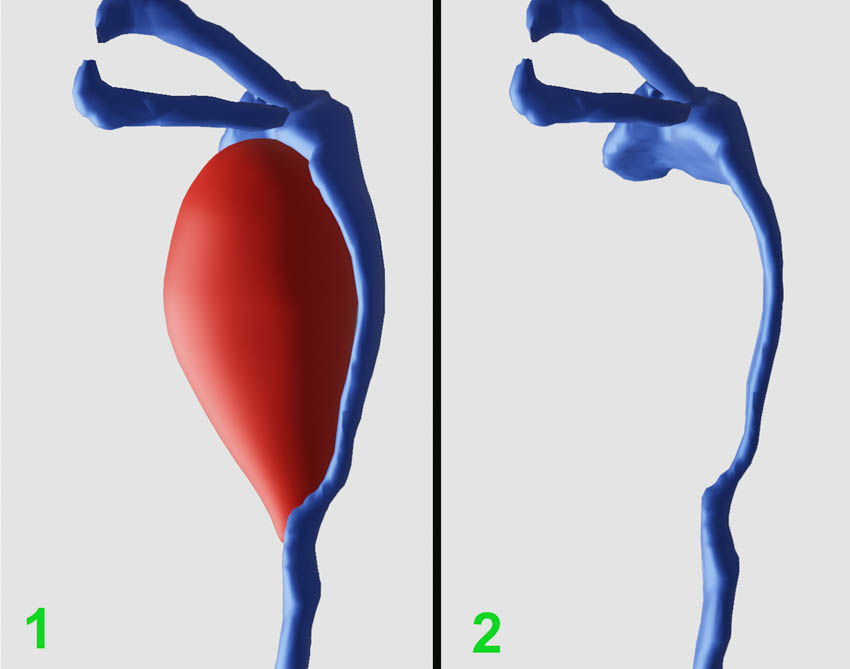
Figure 5. Three-dimensional reconstruction shows relationship of the lesion with the compressed lacrimal system (posterior-anterior view from the back of the left orbit; 1- lacrimal system in blue color, the cyst in red color; 2-isolated, compressed lacrimal system)
Surgical Technique
A curvilinear skin incision was taken to approach the lacrimal sac fossa. The lesion was round to oval, firm with a yellowish surface. The lesion was found to adhere to the anterolateral wall of the lacrimal sac. A probe was placed in the sac, and a careful dissection was performed.
Following the complete excision of the lesion (Fig. 6), a focal area (9 × 6 mm) of the lacrimal sac was found to be injured with loss of tissue. The lacrimal drainage system was first intubated with a Crawford bicanalicular intubation to secure the lacrimal drainage pathway (Fig. 7).
Nasal mucosa was harvested from the floor of the left nasal cavity following a standard decongestion (Fig. 8). The graft was fashioned in a way to deliberately oversize and achieve final dimensions of 12 × 9 mm (Fig. 9). The graft was secured by an end-to-end suturing with 6-0 vicryl (Fig. 2C). Lacrimal irrigation was performed to ascertain no leakage from the sac wound.
Skin wound closure was then closed in a standard way. Histopathological examination was consistent with a diagnosis of a dermoid cyst. The postoperative period was uneventful. Skin sutures were removed at 1 week. Stents were extubated at 3 months.
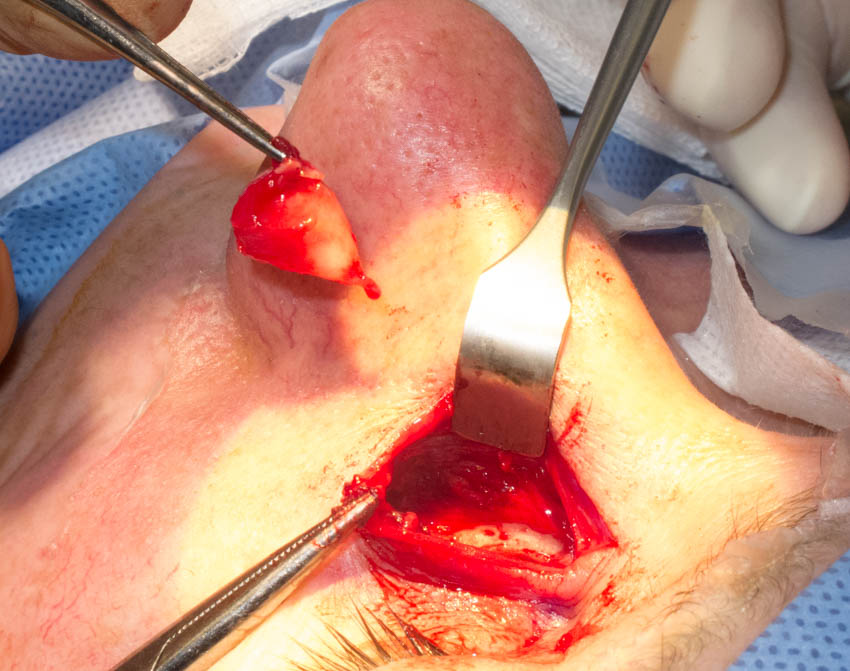
Figure 6. Excision of the cyst

Figure 7. Visible bare silicone stents within the lacrimal sac defect
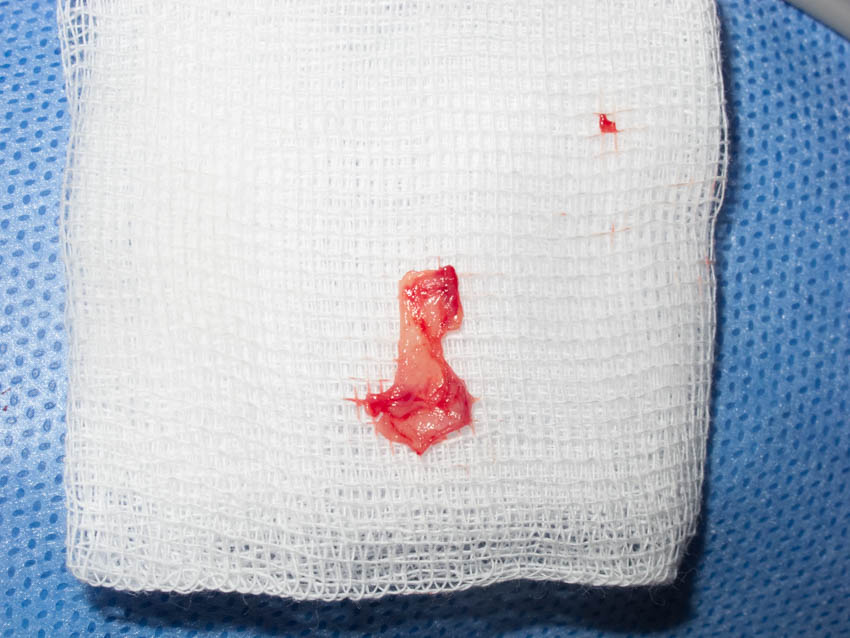
Figure 8. Harvested nasal mucosa

Figure 9. Nasal mucosa graft covering lacrimal sac defect
Follow-up
Epiphora gradually improved over 3 months. Lacrimal irrigation at 3 months was freely patent. A CT-DCG was performed at the 6-month visit, which showed reversal of the lacrimal sac compression with patent lacrimal drainage (Fig. 10).
Although the shape of the lacrimal sac was a little irregular on the CT-DCG, the sac integrity was good. Three-dimensional reconstructions from the postoperative CT-DCG showed good anatomical integrity of the lacrimal drainage system (Fig. 11).
The patient was asymptomatic within the follow-up time of 2 years. Also, the cosmetic effect was excellent (Fig. 12-13).
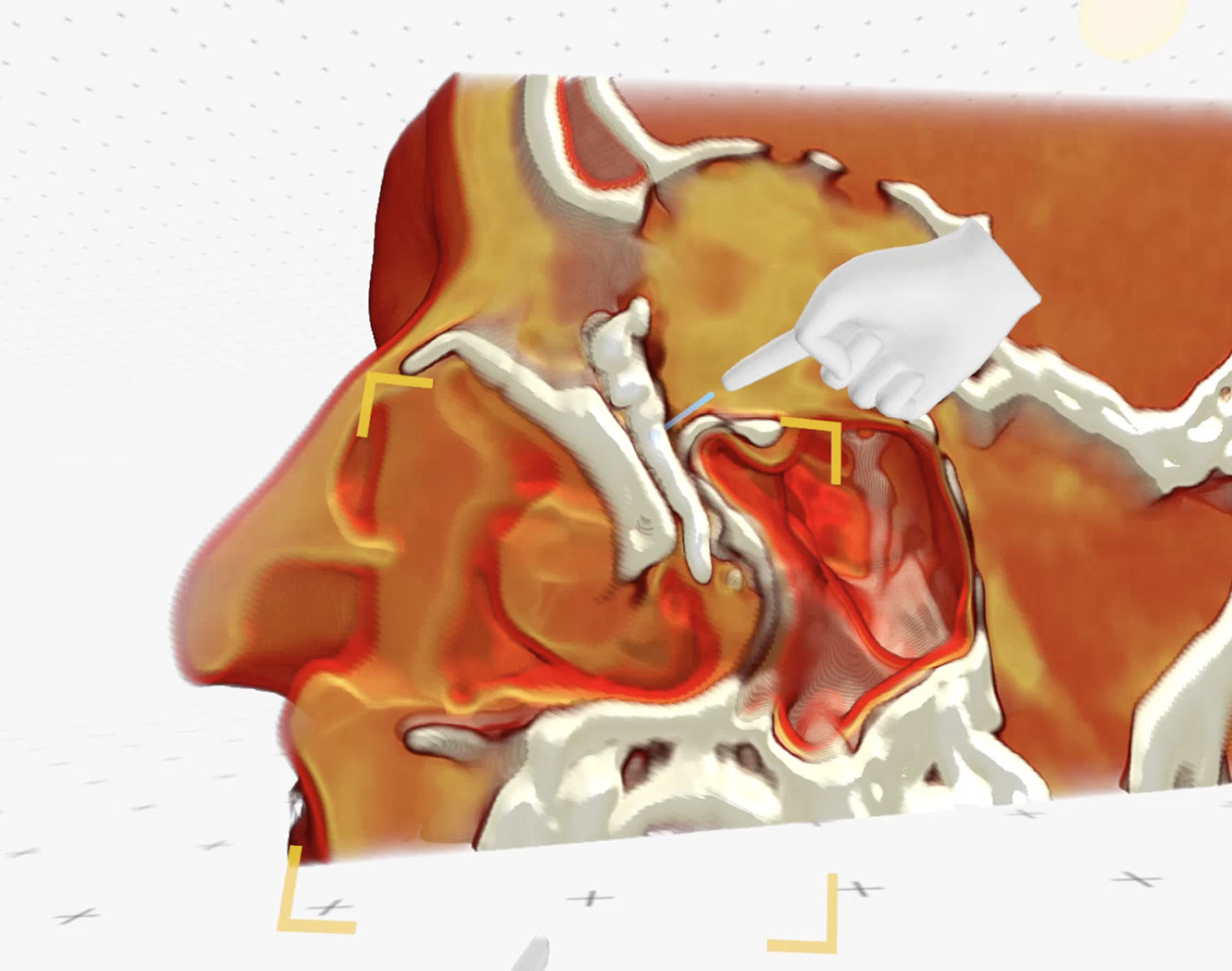
Figure 10. Medical Imaging XR postoperative reconstruction shows well contrasted and filled lacrimal sac and nasolacrimal duct
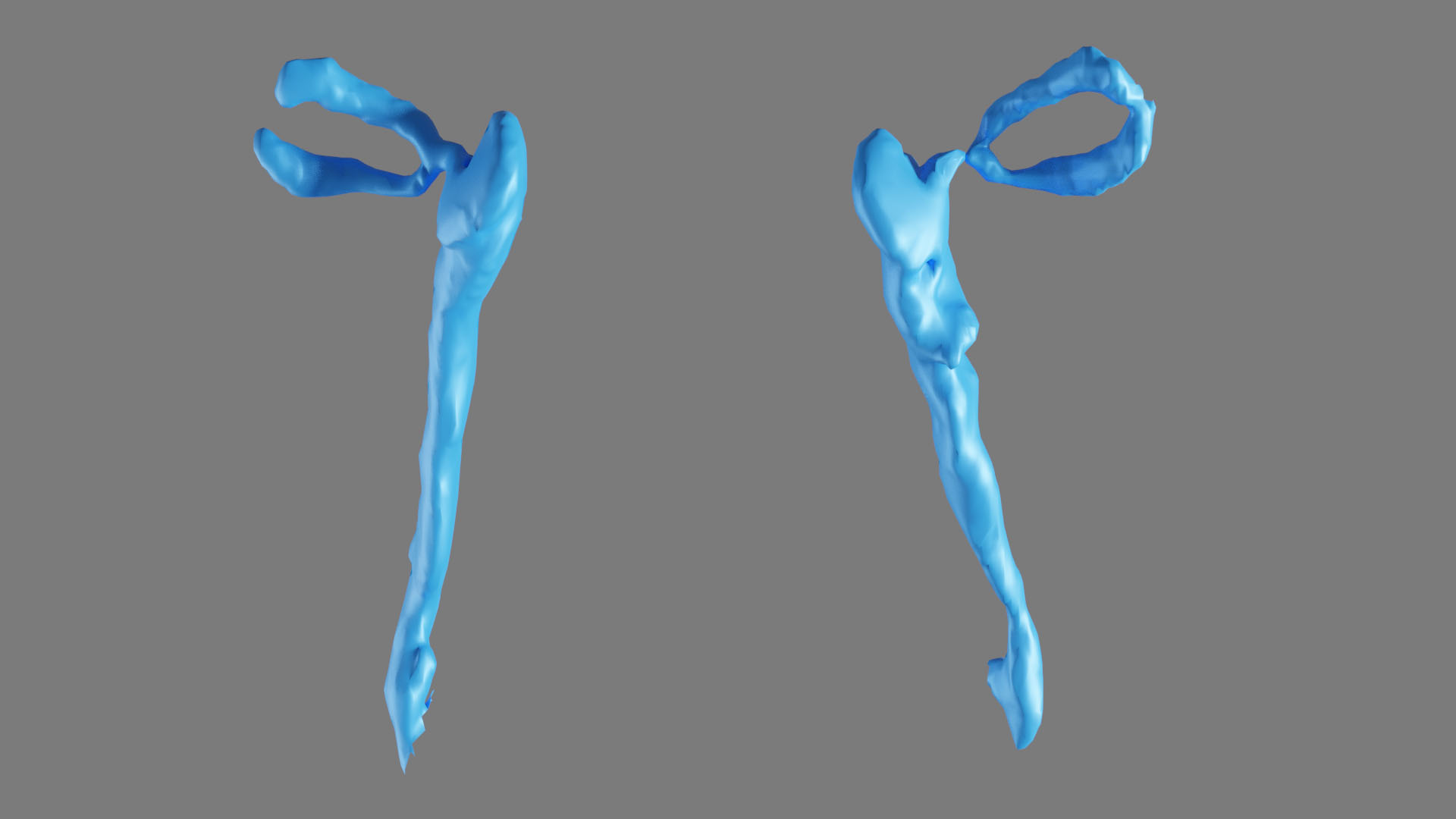
Figure 11. Postoperative three-dimensional reconstruction of the lacrimal system (right – well filled lacrimal system with smooth walls; left – well filled lacrimal system with irregularities within inferior part of the lacrimal sac

Figure 12. Operated area at follow-up after 6 months
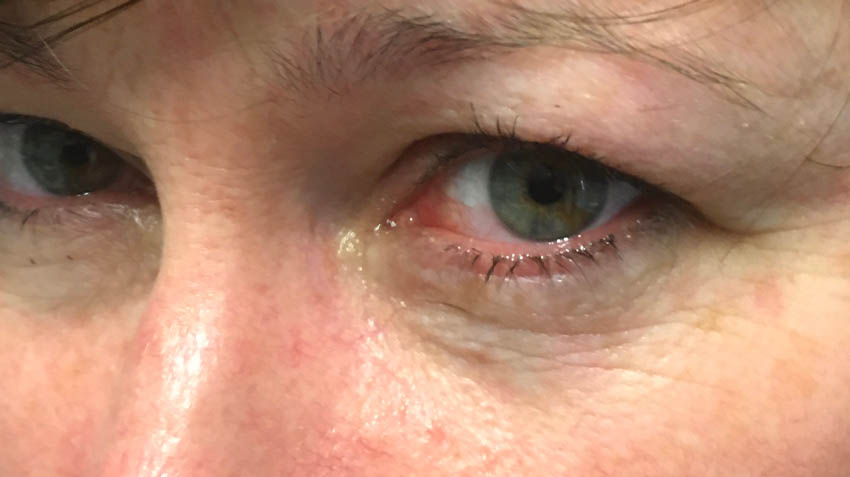
Figure 13. Operated area at follow-up after 1 year
For more information, contact info@medicalholodeck.com February 2023