Development and Pilot Testing of a Collaborative Virtual Reality System for Thoracic Surgery Education. Surgery Open Science 10: 100088.
https://doi.org/10.1016/j.sopen.2024.10.008System design and implementation
A mobile VR system was built using consumer-grade hardware. Five workstations equipped with modern graphics cards and Oculus headsets were mounted in a rollable cabinet, enabling setup anywhere on campus. Each workstation launched Medical Imaging XR, displaying real-time volumetric CT reconstructions as interactive 3D holograms. Students and instructors met together in shared virtual rooms, each participant moving freely around the dataset to examine trauma, infection, or oncological cases from any perspective.
Schematic overview of the VR teaching session.
Teaching procedure
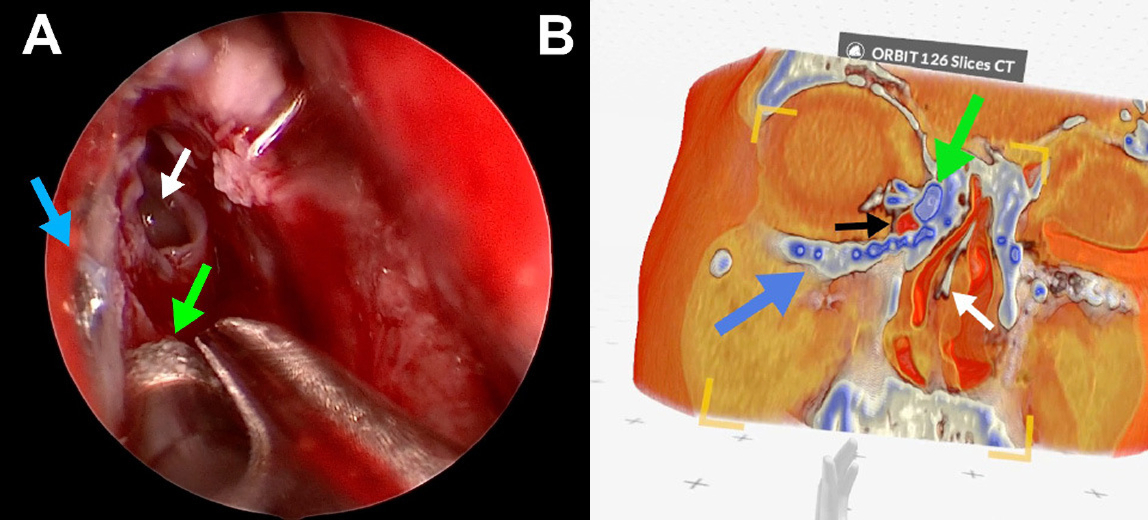
During a two-hour class, small groups of students explored clinical cases including rib fractures with pneumothorax and pulmonary nodules. Lecturers guided the session initially, before handing control to the students for independent exploration. The experience resembled traditional case-based learning, but with the patient’s anatomy fully represented in immersive 3D instead of 2D displays or static plastic models.
Student experience and feedback
Seventy fourth-year students completed the first pilot round. Most had no previous experience with virtual reality, yet 77.14 percent found the system intuitive to use. Cyber sickness was rare, occurring in fewer than 6 percent of participants.
The educational effect was strong: 98.57 percent reported that VR improved their understanding of anatomy compared to conventional methods, and 88.57 percent felt they learned more effectively. The format also delivered high engagement, with 97.14 percent describing the experience as enjoyable.
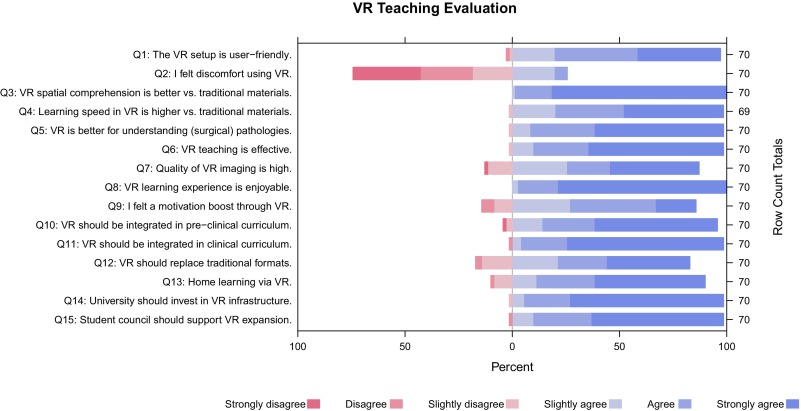
Results of VR teaching evaluation.
Integration and future applications
Students strongly supported integrating VR into the wider medical curriculum. More than 81 percent believed VR has a place in preclinical anatomy courses, while 94.29 percent endorsed its use in clinical training. Many also believed VR could partly replace traditional approaches and enable at-home participation. Over 90 percent encouraged expanding VR infrastructure at the university.
Bridging the gap between theory and practice
This pilot study demonstrates that collaborative, real-time VR teaching is technically feasible using accessible equipment and is well accepted by learners. It offers a way to visualize surgical data spatially, improve anatomical comprehension, and expand teaching capacity without increased physical resource demands.
The immersive experience bridges the gap between theory and practice, allowing students to interact with patient anatomy in ways that were previously possible only in live clinical settings.

Presentation of a serial rib fracture with fragment dislocation (left) and consecutive haemato-pneumothorax (right).
A scalable solution for surgical education
Immersive VR provides a scalable, low-cost solution for graduate surgical education, enhancing understanding, engagement, and spatial reasoning. Future studies will measure objective learning outcomes and explore broader integration into medical curricula, including asynchronous and at-home learning.
The project sets a precedent for using collaborative VR as a standard component of surgical education, combining accessibility, interactivity, and immersive technology to improve graduate training.
For more information, contact info@medicalholodeck.com November 2025