In a recent publication in KSSTA, the authors demonstrated that XR technologies significantly enhance orthopedic training, intraoperative precision, and rehabilitation outcomes.
XR technologies in healthcare and orthopedics
In healthcare, XR technologies are transforming the way medical practice operates by connecting virtual and real-world environments, reshaping medical education, improving procedural precision, and enhancing patient care. For example, VR simulators have proven effective in helping clinicians develop surgical skills while reducing the risks linked to early hands-on clinical experience and eliminating the need for cadaver-based training.
Within orthopedic surgery specifically, AR navigation systems enhance procedural accuracy in total knee and hip arthroplasty by improving component alignment and reducing intraoperative errors, which may lead to improved long-term patient outcomes.
Digital twins and AI in orthopedics
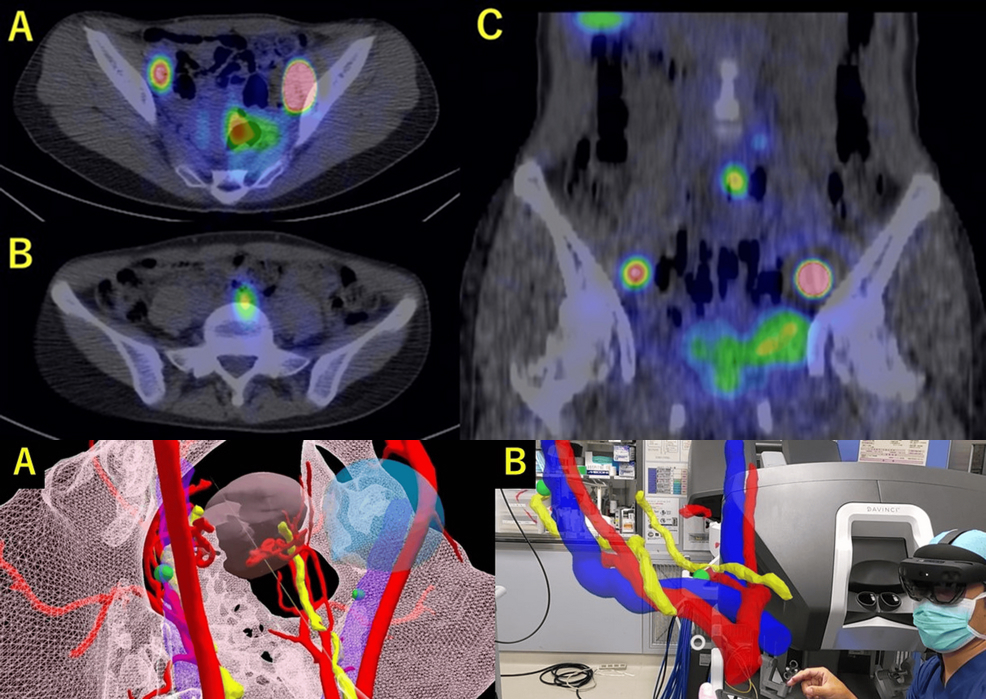
Among these advancements, digital twin technology appears as an innovative application of XR in orthopedics, enabling personalised surgical planning, real-time rehabilitation monitoring, and predictive modeling of musculoskeletal disorders by combining multiple data sources with computational simulations.
Alongside these XR developments, large language models like ChatGPT and emerging multimodal AI systems such as DeepSeek are shaping orthopaedic research by improving accessibility to medical language, simplifying manuscript preparation, and providing innovative tools for clinical decision-making and literature review.
Integrating AI into XR platforms has the potential to further enhance orthopedic surgery by enabling personalized predictions and supporting surgical training.
XR in sports traumatology and arthroscopy
In the field of sports traumatology and arthroscopic surgery, XR technologies offer clear and clinically meaningful advantages.
VR-based arthroscopy simulators enable trainees to repeatedly practice shoulder and knee procedures in safe, controlled settings, speeding up skill acquisition while reducing risk.
During surgery, AR-guided navigation can improve tunnel placement in ACL reconstructions, decrease fluoroscopy use during multiligament repairs, and enhance visualization in complex shoulder operations.
After surgery, virtual and AR-based rehabilitation tools promote patient adherence, allow for remote monitoring, and support more efficient decisions regarding return-to-sport readiness.
Scope and objectives of the review
This review provides a clinician-oriented perspective on how XR integration can enhance procedural outcomes, patient safety and accessibility in orthopedic care. It’s focused on three pillars:
-
Immersive surgical education and VR simulation
-
AR/MR-enhanced surgical procedures
-
Rehabilitation
Orthopedic surgical training with immersive technologies

The idea of using VR-based simulators for surgical training emerged from the observation that surgeons with video gaming experience adapted more rapidly to tasks involving indirect visualization and precise motor coordination, especially in arthroscopic and laparoscopic procedures.
VR simulators provide trainees with the opportunity to practice a wide range of skills - from anatomical dissections to intricate surgeries like arthroscopy, fracture repair, and arthroplasty - within safe, controlled, and risk-free environments.
VR simulator types and benefits
Screen-based VR simulators
These systems combine physical models, haptic feedback, and high-resolution screens. They typically use tracked instruments but do not rely on VR headsets.
-
Applications: knee and shoulder arthroscopy.
-
Benefits: improved hand - eye coordination and procedural accuracy.
-
Some platforms include haptic feedback, providing tactile resistance to help trainees understand tissue handling, force application, and instrument control.
Fully immersive headset-based VR simulators
These use VR headsets and hand controllers to create a fully virtual training environment.
-
Applications: arthroscopy, fracture fixation, deformity correction, arthroplasty.
-
Applications: arthroscopy, fracture fixation, deformity correction, arthroplasty.
-
Additional advantage: real-time collaborative sessions with participants worldwide, enabling global surgical education.
AR and MR in surgical training
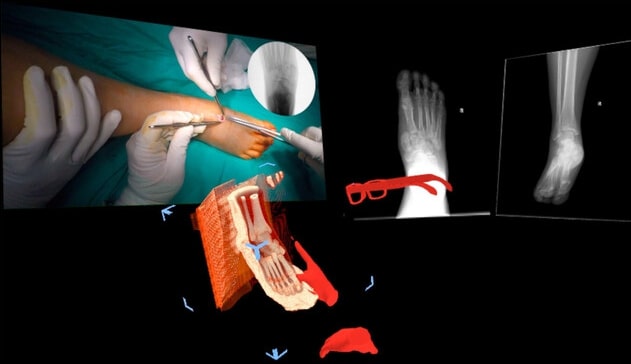
AR and MR require specialised devices to integrate virtual components into real-world settings, including position trackers and head-mounted displays. These devices allow intraoperative image guidance, data monitoring and surgical training, despite limitations such as low pass-through resolution. AR enhances trainee engagement, provides real-time feedback, and enables hands-free guidance and remote mentorship.
Potential of the metaverse in surgical education
The so-called metaverse offers benefits such as increased student engagement, safe decision-making environments, gamification and blockchain verification. Future virtual training could evolve into highly realistic and complex simulations, potentially becoming integral to orthopedic curricula. Challenges include digital access disparities, high device costs, and platform fragmentation.
Applications in orthopedic surgery
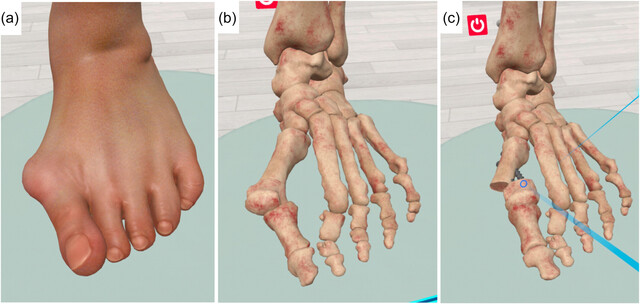
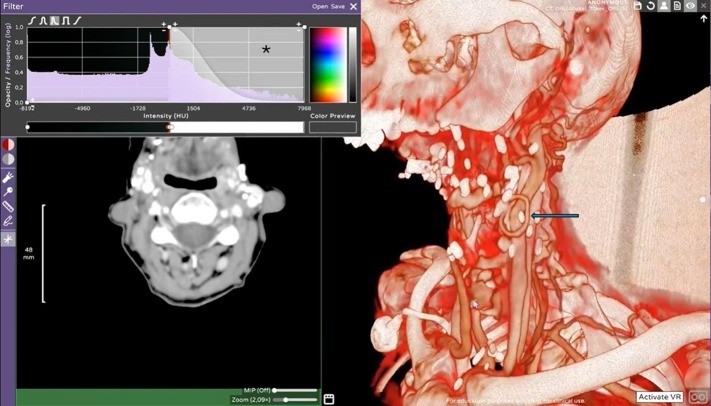
VR and AR have transformed preoperative planning, intraoperative navigation, and postoperative rehabilitation. VR enhances surgical precision and planning, while AR improves intraoperative guidance, implant positioning, and visualisation.
The table below summarises key applications across surgical phases, demonstrating the distinct clinical value of XR technologies in fracture fixation, arthroscopy, and arthroplasty.
Integration of AI with XR in surgery
When combined with AI and VR/AR, XR technologies can provide adaptive solutions for surgical planning and decision-making, assist training, and bridge the experience gap between novice and expert surgeons. Challenges include ethical concerns regarding patient data and limited AI performance in rare or data-scarce situations.
XR in musculoskeletal rehabilitation
XR-based rehabilitation extends care beyond clinical settings through telemedicine and wearable devices like IMUs, allowing continuous monitoring of joint motion and gait. VR provides fully immersive environments, while AR overlays virtual guidance onto real-world exercises. Studies demonstrate improved compliance, functional recovery, pain reduction, and effectiveness comparable to in-person physiotherapy.
Future directions and research needs in rehabilitation
XR rehabilitation has also been applied to chronic disorders, acute pain management, and phantom limb pain. As XR applications expand, future research should optimize protocols, tailor interventions, and assess long-term outcomes to establish clinical effectiveness in routine orthopedic practice.
Towards personalized and predictive orthopedic care
XR technologies are becoming integral to orthopedic practice, bridging the gap between education, surgery, and rehabilitation. VR simulators accelerate skill development in safe environments, AR and MR enhance intraoperative precision, and XR-based rehabilitation tools extend care beyond the clinic. With the added potential of AI and digital twin integration, these technologies promise more personalized, predictive, and efficient orthopedic care.
For more information, contact info@medicalholodeck.com September 2025