The limitations of 2D medical imaging
Nowadays, as medical treatments become more complex, the shortcomings of 2D imaging have become increasingly clear.
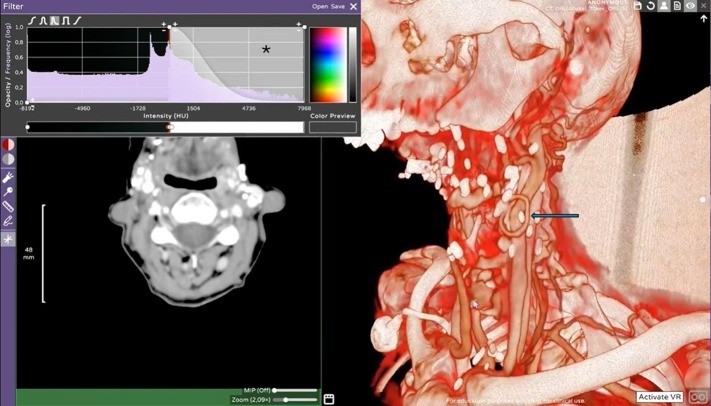
A primary challenge is the loss of spatial context. Clinicians must mentally reconstruct three-dimensional anatomical structures from multiple cross-sectional slices. This mental integration increases the risk of misinterpretation, particularly when dealing with unusual anatomy, overlapping structures, or subtle pathological findings.
2D imaging also hides relationships between structures. Surgeons may know a tumor’s position in theory, but without depth perception, it’s harder to judge how close it is to a vital vessel or nerve. Even with multiple views, essential details can remain ambiguous until the patient is on the operating table - when mistakes are costliest.
Flat scans can be a barrier to communication. Patients, trainees, and even specialists from other disciplines may struggle to interpret them, which can lead to misunderstandings, slower decision-making, and, in some cases, errors in treatment planning.
What is spatial imaging?
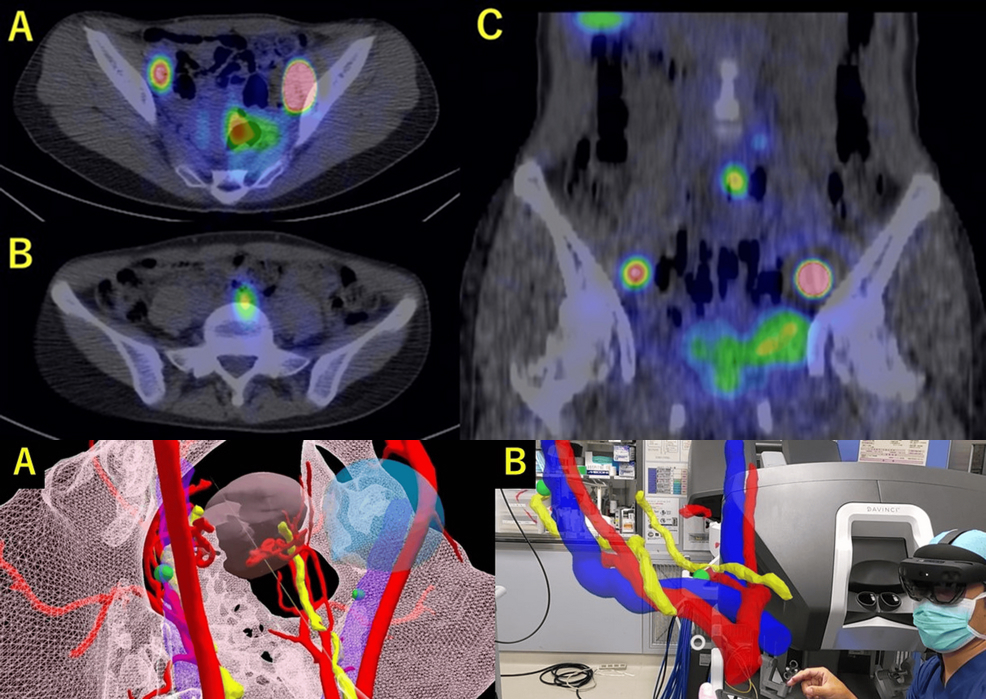
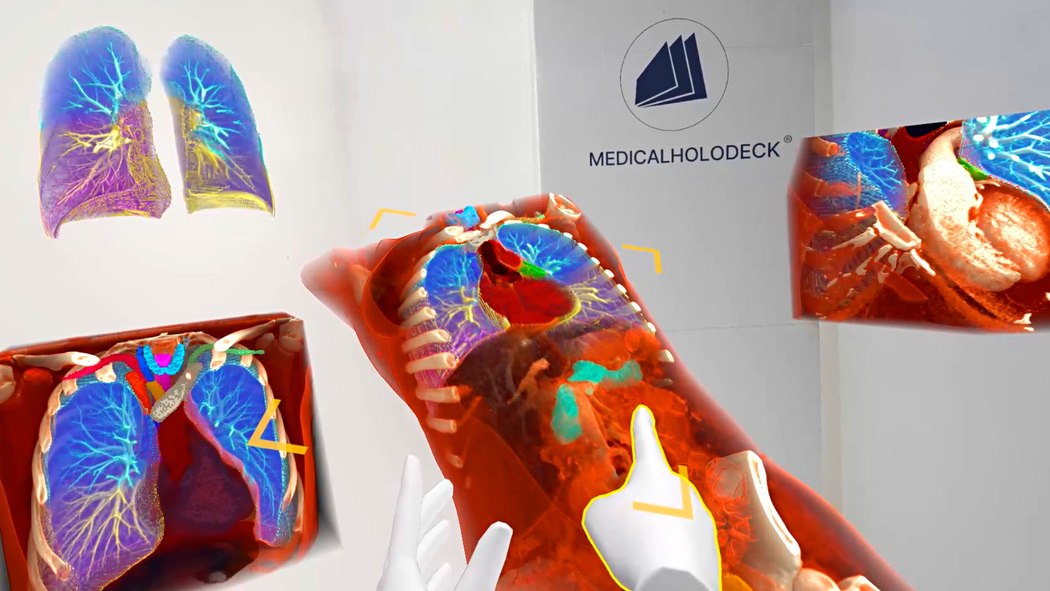
Spatial imaging transforms traditional medical scans, like CT or MRI into fully interactive, three-dimensional representations of anatomy and pathology. This technology enables clinicians to step inside a virtual space, rotate the model, zoom in on fine structures, and view the anatomy from any angle.
This means converting real patient data into immersive environments where tissues, bones, and organs are presented in their true scale and spatial relationships.
Seeing anatomy in true scale and context
In a virtual 3D environment, anatomy is displayed in true scale. A surgeon can instantly measure the exact distance between a tumor and a major artery, or see how a fracture disrupts surrounding bone structures. Rotating the model, slicing it along any axis, or virtually exploring the anatomy reveals relationships that are nearly impossible to detect in flat images.
This spatial awareness translates directly into better decision-making. Whether preparing for a delicate neurosurgery or mapping the safest path for a catheter, the ability to view patient anatomy as it truly exists in space helps eliminate guesswork - and the costly surprises that often come with it.
Better diagnosis and surgical planning
Spatial imaging offers a virtual rehearsal space. Procedures can be planned step by step, testing different approaches and anticipating challenges before entering the operating room. This preoperative simulation not only increases surgical precision but also shortens procedure times, reduces patient risk, and improves overall outcomes.
Even in multidisciplinary teams, planning becomes more efficient. Radiologists, surgeons, and other specialists can gather in the same virtual environment, view the same structures, and agree on the best course of action - removing the communication gaps that sometimes lead to errors or delays.
Collaboration without borders

Clinicians now can enter the same virtual space from anywhere in the world and examine identical, interactive 3D models in real time. This borderless collaboration accelerates decision-making and broadens access to expertise. Rural hospitals can connect with leading specialists instantly, and complex cases can be reviewed without the delays of physical travel or shipping data between institutions.
Empowering patient communication
By showing patients a true-to-scale, interactive 3D model of their own anatomy, clinicians can visually explain where a problem is, how it affects surrounding structures, and what the planned treatment will involve. Instead of relying on complex medical terminology, doctors can rotate, zoom, and dissect the model in real time, making the information accessible to any level of health literacy.
This visual, hands-on approach not only improves patient understanding but also builds trust. When patients can see exactly what is happening inside their body, they are more likely to ask informed questions, feel confident in the proposed plan, and actively participate in decisions about their care.
The clinical shift from 2D imaging to spatial 3D
2D imaging often lacks spatial context, forcing clinicians to mentally reconstruct anatomy and increasing the risk of mistakes. Spatial imaging eliminates these limitations by converting CT, MRI, and other scans into interactive 3D models that display anatomy in true scale and context.
It allows for more precise diagnoses, virtual surgical rehearsals, and improved preoperative planning, reducing patient risk and enhancing outcomes. It also fosters seamless collaboration among multidisciplinary teams and enables remote experts to analyze the same data in real time.
Beyond professional use, spatial imaging empowers patients by turning complex scans into understandable visualizations, strengthening trust and shared decision-making.
For more information, contact info@medicalholodeck.com September 2025