Quality teaching is always a challenge and must evolve as new tools become available. At the Medical Faculty, University Hospital Bonn, Germany, a collaborative, multiuser VR system was developed to enhance thoracic surgery education. The study evaluated the feasibility and acceptance of a fully interactive, case-based VR program for graduate surgical students, demonstrating high usability, improved anatomical understanding, and strong engagement.
Feodorovici P, Sommer N, Bergedieck P, Lingohr P, Kalff JC, Schmidt J, Arensmeyer JC. (2024) Development and Pilot Testing of a Collaborative Virtual Reality System for Thoracic Surgery Education. Surgery Open Science 10: 100088. doi:10.1016/j.sopen.2024.10.008
https://www.surgopensci.org/article/S2589-8450(24)00130-1/fulltext
Bridging theory and practice with VR
Each patient presents a unique and complex pathology, making it crucial for medical students to learn how to extract and apply knowledge effectively. Case-based learning (CBL) focuses on the patient’s story and is a cornerstone of modern medical education.
Traditional methods like textbooks, models, and cadavers are limited by their static, 2D nature, while videos and online resources cannot fully convey 3D anatomy. VR offers an immersive, interactive way to explore realistic anatomy and surgical scenarios, bridging the gap between theory and practice.
This article describes the development and pilot of a collaborative VR system that uses real-time CT data to teach surgical cases, evaluating its feasibility and educational impact.

VR infrastructure
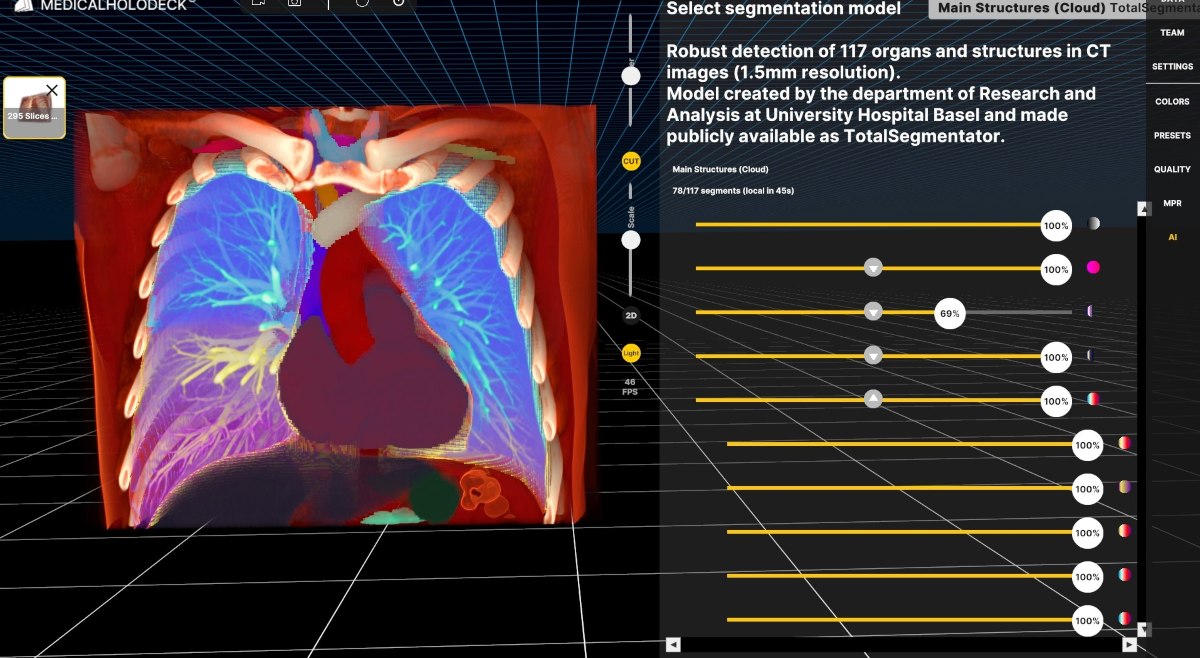
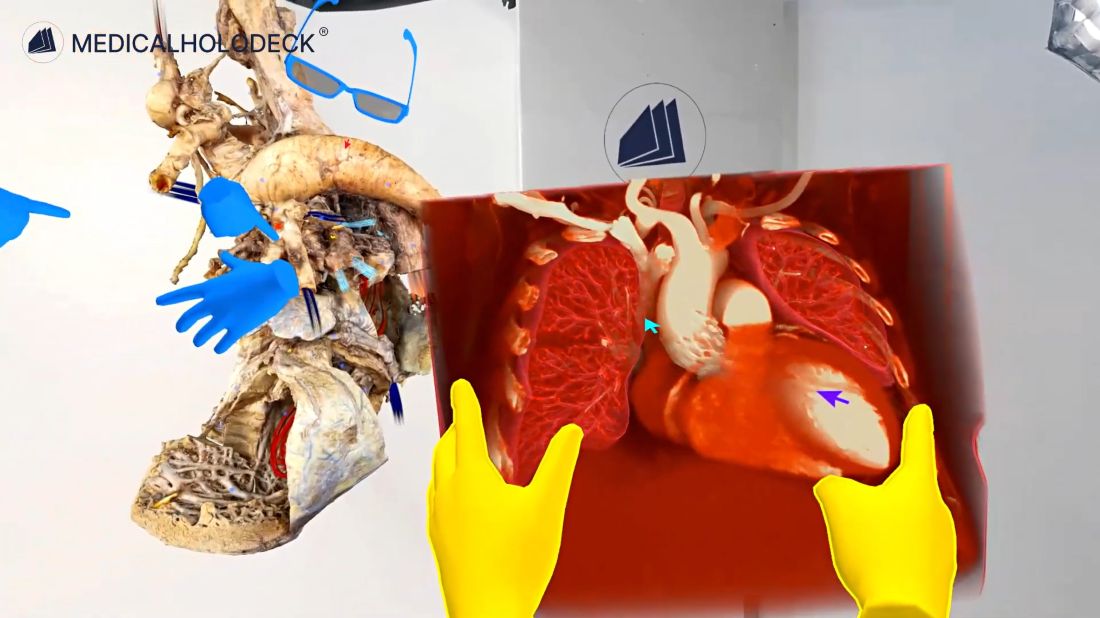
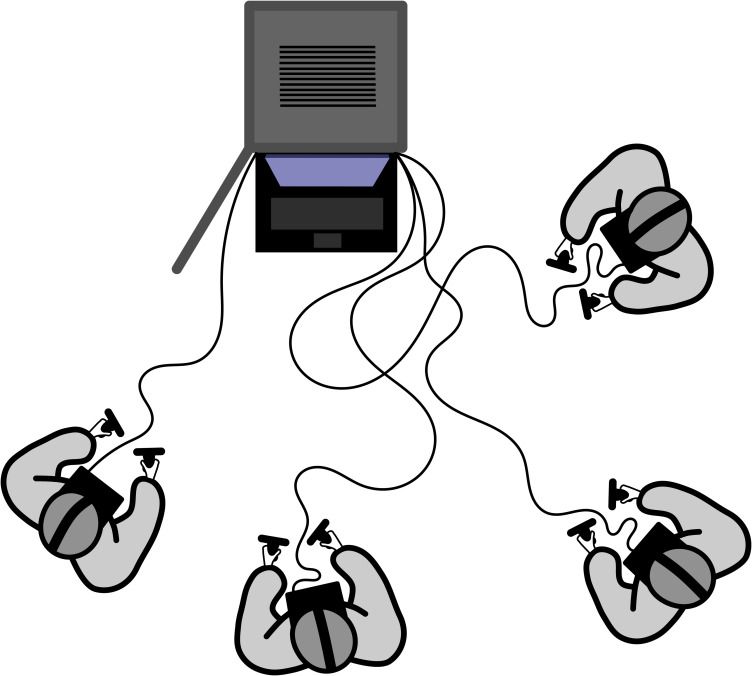
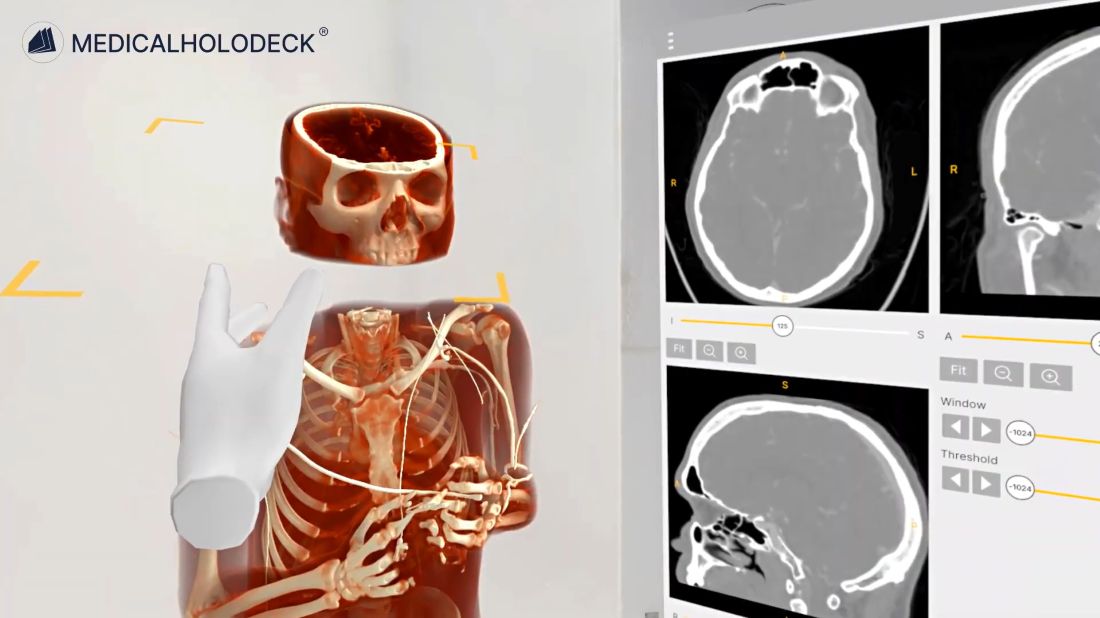
The system, built in late 2019, used five high-performance workstations with Oculus Rift-S HMDs for immersive VR. Users interacted with 3D patient images in a collaborative virtual room using Medical Imaging XR (Medicalholodeck) software, manipulating them with controllers. CT datasets were processed and saved as interactive 3D visualizations for case-specific surgical teaching.
Immersive VR for surgical training
The study involved fourth-year medical students at the University of Bonn taught by trained surgical residents.
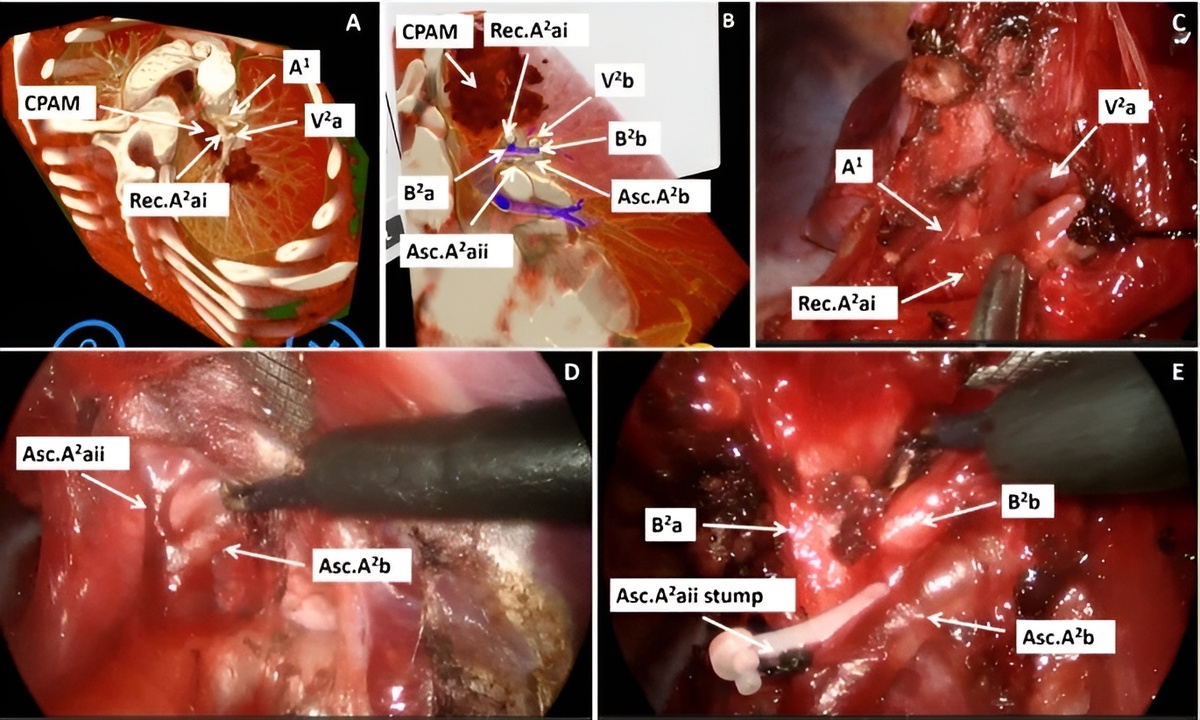
The curriculum featured CT scans of five representative thoracic surgery cases, including rib fractures leading to a haemato-pneumothorax and a pulmonary nodule in the right lower lobe.
The 2-hour VR session for 8–10 students began with a 10-minute introduction on the technology and equipment, after which students were divided into small groups of 2–3. The teacher guided the group through predefined 3D curricula of various pathologies, with students initially observing and interacting via virtual “laser pointers” while seeing each other in the virtual space. At the end, students were given full control to freely explore and interact with the 3D reconstructions.
Student feedback on VR training
After each VR session, participants completed a 15-question Likert-scale survey assessing usability, visualization, learning, and cyber sickness.
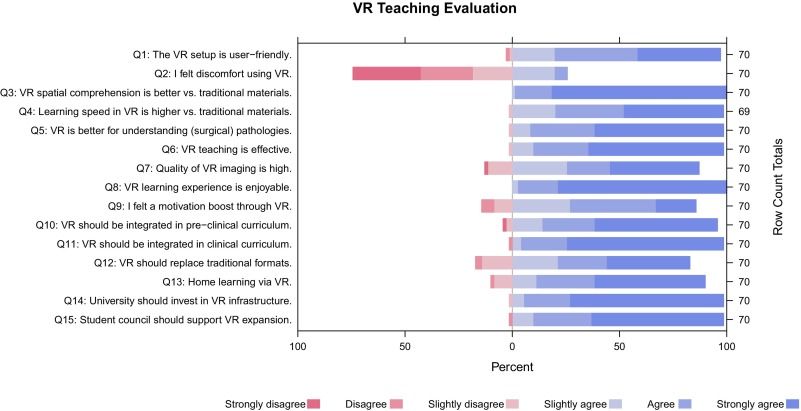
The VR setup was rated highly intuitive and user-friendly, with minimal reports of cyber sickness. Most students agreed that VR enhanced their understanding of anatomy, surgical pathologies, and spatial relationships, and found it enjoyable and effective. Support for integrating VR into preclinical and clinical teaching was strong, and many expressed interest in future VR courses at home. Comments praised the visualization quality and engagement, while noting minor issues with interface complexity and spatial positioning.
Implementing VR in medical teaching
A real-time VR program for teaching gross anatomy and surgical pathology has been successfully demonstrated, showing technical feasibility and strong student acceptance. Two follow-up studies will assess its educational impact, while potential drawbacks - like reduced in-person learning - must be carefully addressed as VR use expands.
Enriching medical teaching with Medicalholodeck improves students’ spatial understanding and engagement. This innovative approach makes learning more accessible and interesting, and can enhance medical education with immersive, interactive environments.