Immersive visualization for complex cases
Chronic pain procedures like peripheral nerve stimulation (PNS), nerve blocks, and intrathecal pump placements require detailed anatomical understanding. This becomes particularly complex in patients with tumors, altered anatomy, or prior surgeries. In these situations, conventional 2D imaging often falls short. That’s where VR steps in.
By converting standard CT and MRI scans into 3D patient-specific models using Medicalholodeck’s AI-powered software, clinicians were able to examine anatomy in full immersive space, plan precise procedural trajectories, and minimize risk. In six selected patient cases, VR pre-planning helped guide successful procedures – even in previously failed or high-risk interventions.
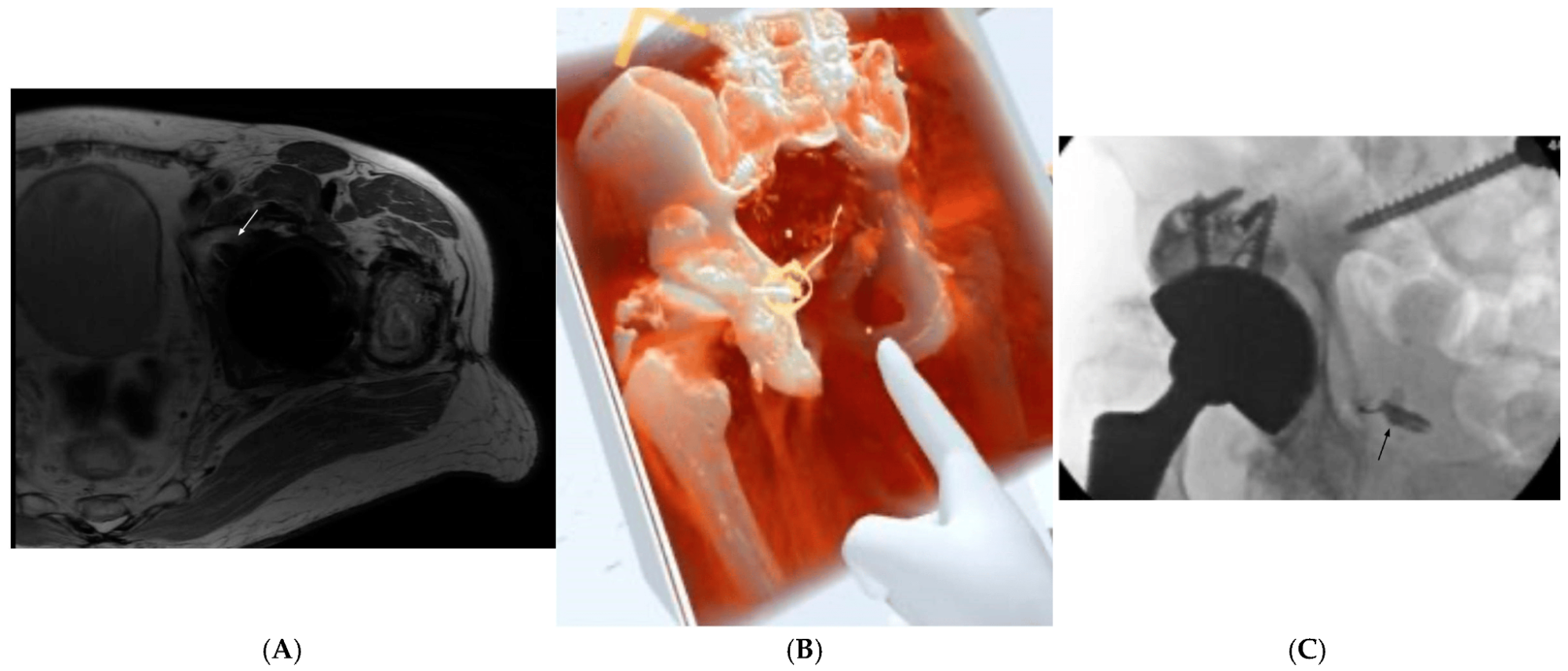
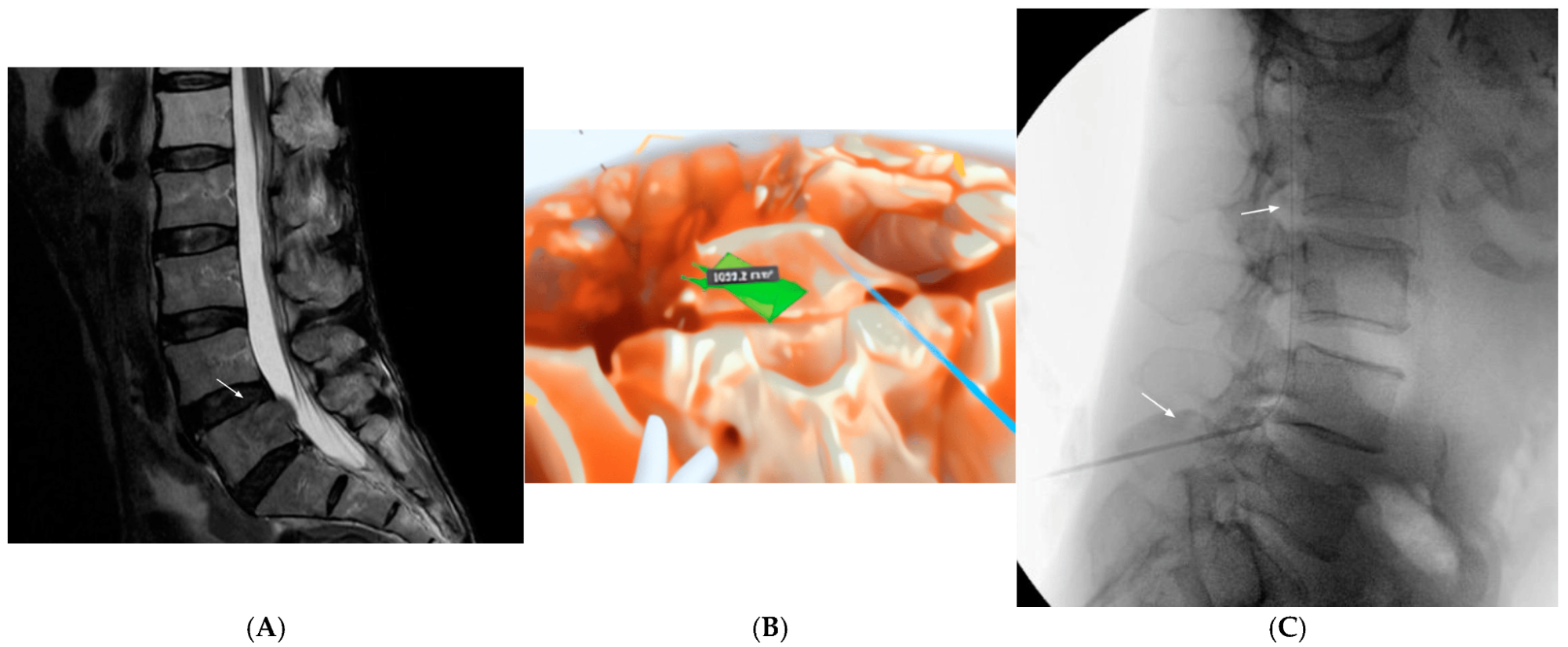
Patient 2 with nerve pain after hip surgery: (A) MRI shows a screw pressing on a nerve area in the pelvis; (B) After the screw was removed, 3D images helped plan how to reach the nerve since a key landmark was missing; (C) Final image shows successful delivery of pain medication to the nerve.
Medicalholodeck in action
From 2022 to 2024, the team used Medicalholodeck’s volumetric reconstruction platform Medical Imaging XR, to automatically segment DICOM files and build full 3D patient models for in-VR review. These models allowed proceduralists to:
-
Visualize and manipulate complex anatomies
-
Measure angles and distances in real scale
-
Identify safe needle and lead paths
-
Plan alternative approaches when prior interventions failed
The segmentation engine behind Medicalholodeck is based on the nnU-Net framework, trained on diverse CT datasets for high accuracy across clinical scenarios. Clinicians could further refine segmentations and annotate areas of interest.
Patient 3 with cancer-related pain who could not tolerate opioids received an intrathecal pump: (A) MRI shows a bone lesion at the L5 vertebra; (B) 3D imaging helped plan the safest path for catheter placement around the tumor; (C) Final image shows the pump catheter correctly positioned through the L3/4 area.
Case highlights
-
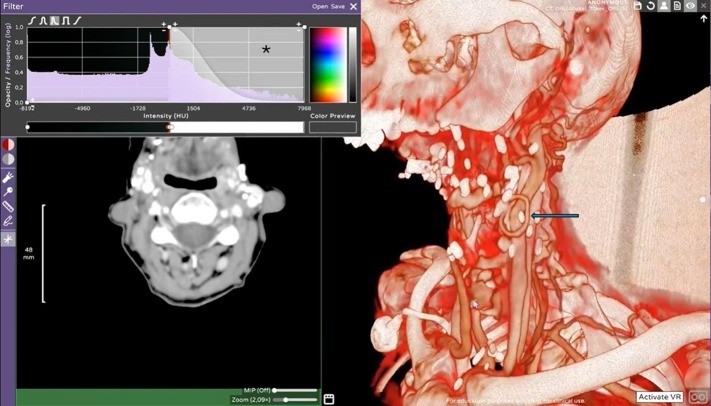
Case 1: A patient with extensive cervical hardware and kyphosis underwent PNS placement. VR helped identify a safer approach, avoiding complications from hardware obstruction.
-
Case 2: After removal of a pelvic screw, a key fluoroscopic landmark was missing. VR allowed a 3D reconstruction to plan a successful pudendal nerve block despite altered anatomy.
-
Case 3: In a cancer patient with spinal metastasis, VR helped plan intrathecal pump placement by assessing tumor margins and safely identifying an access point.
-
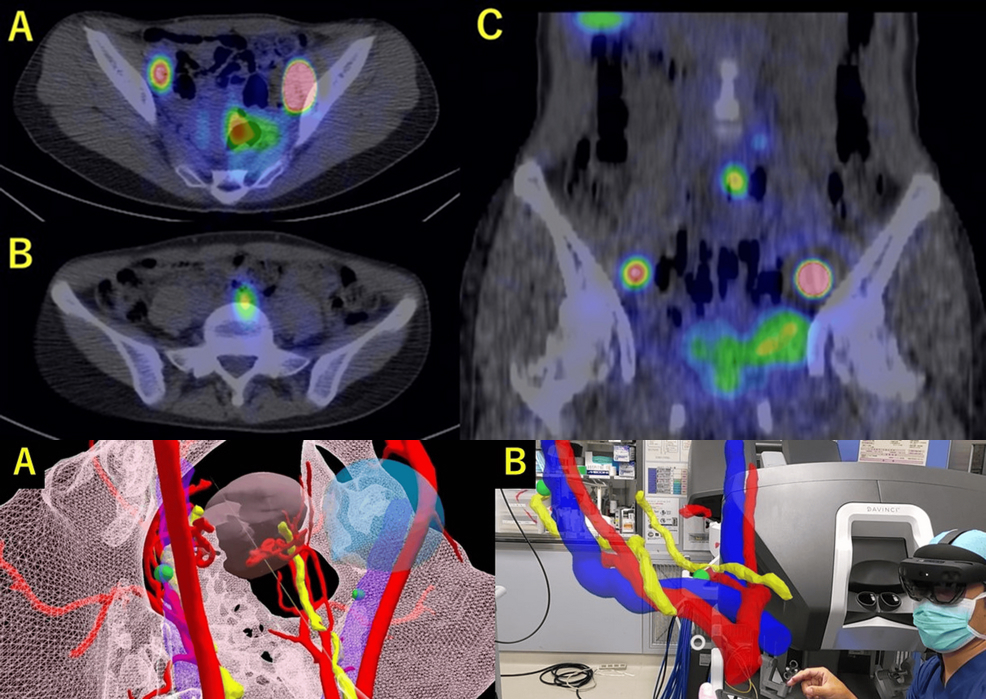
Case 4: A lymphoma patient was evaluated for neuromodulation. VR modeling revealed that epidural lead placement would be unsafe, prompting a switch to peripheral nerve stimulation.
-
Case 5: Following abdominal surgery and muscle atrophy, VR planning helped guide PNS lead placement to treat chronic pelvic pain without damaging adjacent structures.
-
Case 6: For a sarcoma patient with limited respiratory function, VR helped identify a safe zone for a sciatic nerve block above tumor margins – relieving pain and enabling chemotherapy.
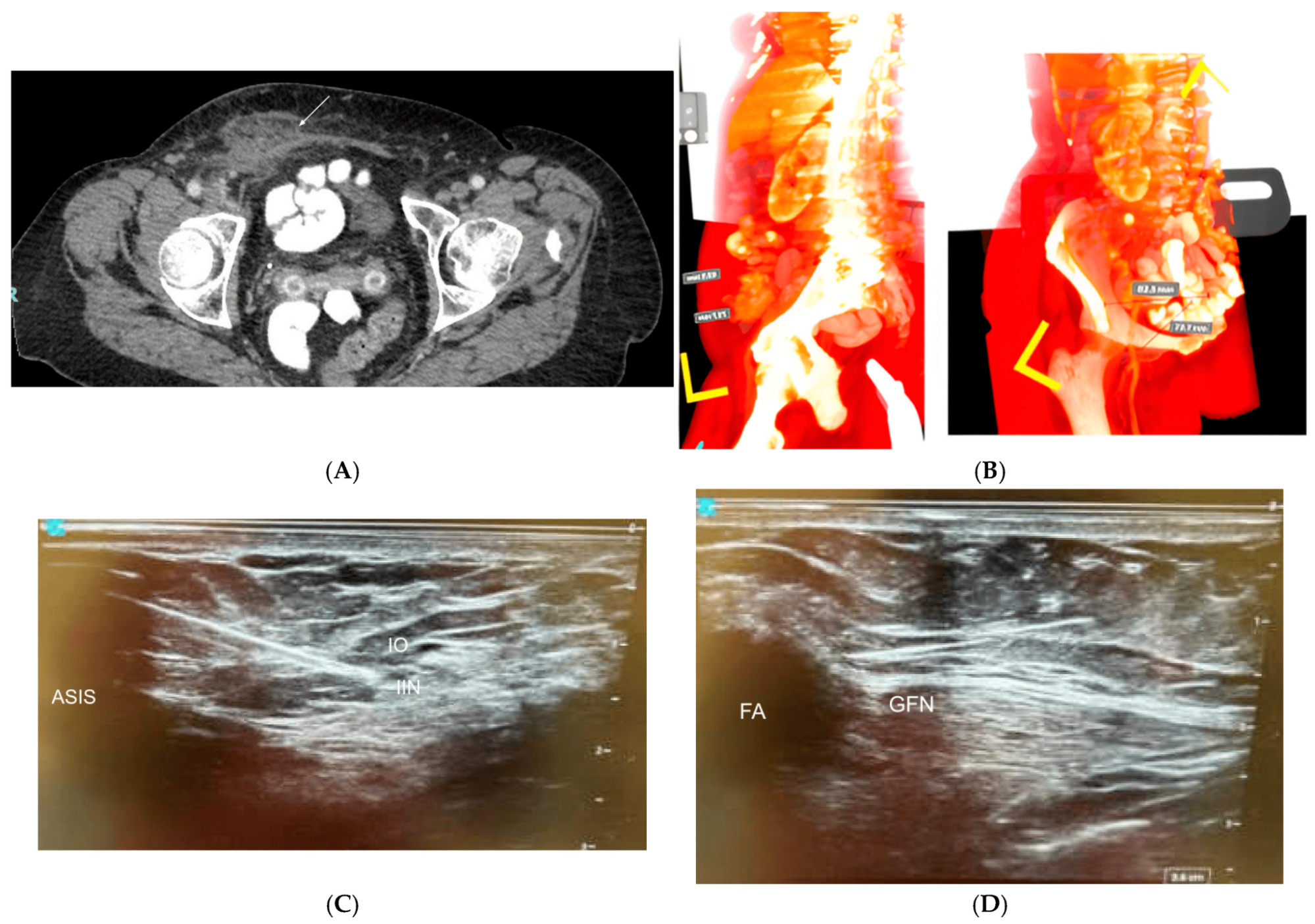
Patient 5 treated with peripheral nerve stimulation (PNS) for chronic abdominal wall pain: (A) CT scan shows fluid buildup near a previous hernia repair; (B) 3D imaging was used to plan the best path for placing the leads; (C) Ultrasound-guided placement of leads near the ilioinguinal and iliohypogastric nerves; (D) Additional lead placement near the genitofemoral nerve.
Why VR works
Unlike flat imaging, VR gives clinicians the spatial awareness needed to navigate complex cases. In this case series, it allowed for:
-
Better procedural accuracy
-
Enhanced decision-making
-
Reduced intraoperative uncertainty
-
Improved patient outcomes
Notably, VR also supported collaborative planning – teams reviewed models together in the virtual environment to explore options and make informed decisions.
AI + VR: a perfect match
The cases showed that automatic segmentation significantly reduced model creation time. While manual segmentation (using tools like Elucis) offered greater detail for complex cases, Medicalholodeck’s AI-powered approach delivered high-speed, high-quality results ideal for routine planning. The ability to switch between automatic and manual methods gave clinicians flexibility based on the case complexity.
What this means for pain management
This series demonstrates a new paradigm in interventional pain procedures. As VR becomes more accessible and easy to use, clinicians can apply it to:
-
Plan safer interventions
-
Explore options in previously failed procedures
-
Educate patients using their own 3D models
-
Build trust through visual, collaborative planning
VR isn’t just for training anymore. It’s being used today by clinicians in real-world hospitals to improve care – backed by measurable outcomes.
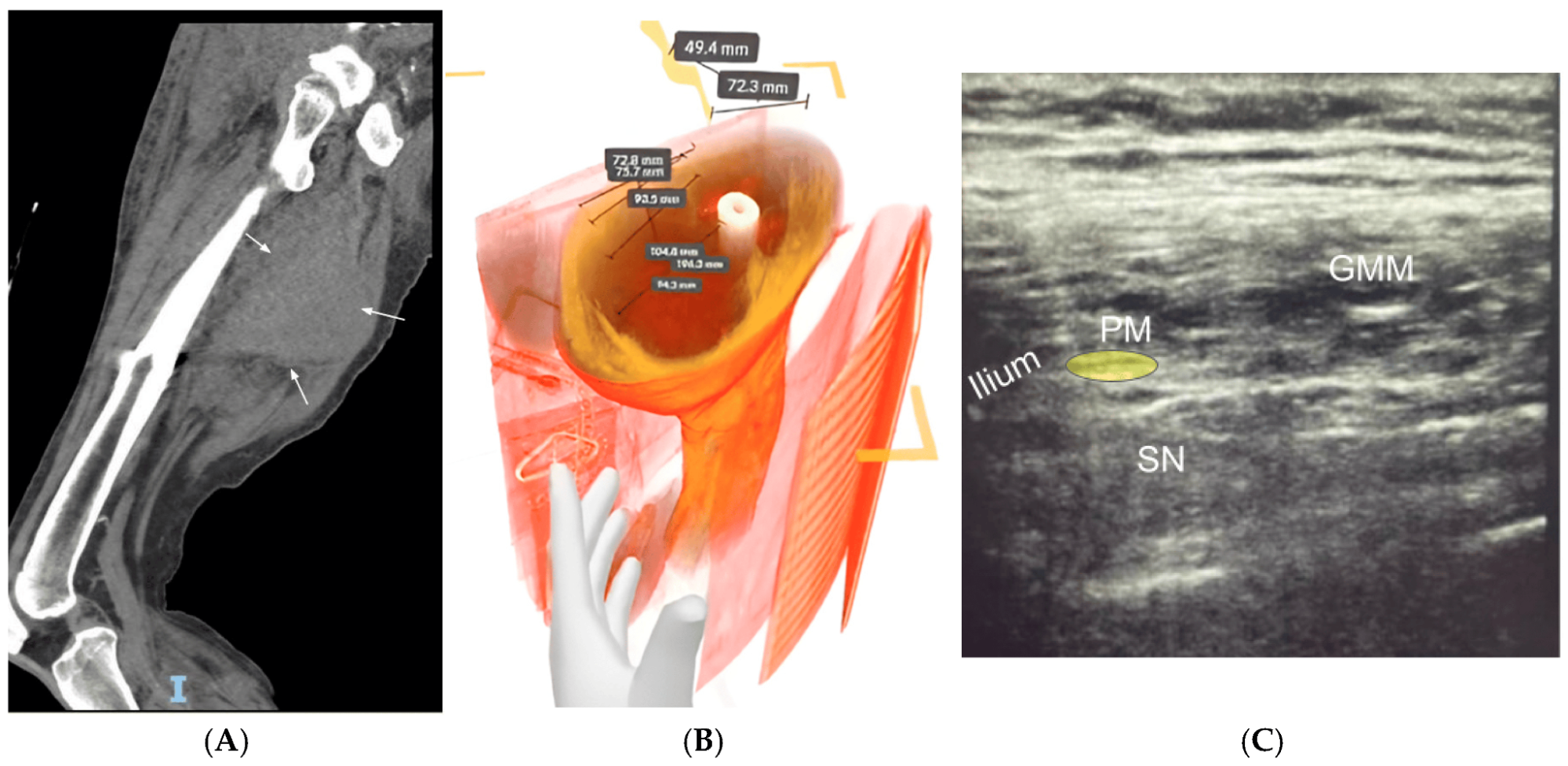
Patient 6 with sciatic nerve pain caused by a large tumor in the thigh muscles: (A) CT scan shows the tumor pressing on much of the sciatic nerve; (B) 3D imaging was used to measure the tumor and plan a safe injection route above it; (C) Ultrasound-guided nerve block was successfully performed above the tumor near the piriformis muscle.
Built with Medicalholodeck
Medicalholodeck’s XR platform enabled four of the six cases in this study, using standard CT/MRI data and a Meta Quest headset. Whether you’re planning a nerve block, mapping out electrode placement, or visualizing tumor proximity, our tools bring patient data into immersive space for more informed decisions.
Explore how Medicalholodeck can help your team:
-
Create 3D models in minutes
-
Segment anatomy with AI
-
Visualize in immersive VR/AR
-
Train procedures with more precision
Start your free trial today – and bring your work into the third dimension. Download your free trial here.
For more information, contact info@medicalholodeck.com May 2025